The evaluation of the shear bond strength between various Hybrid CAD/CAM restorative materials and repairing composite resins
Abstract
The purpose of this study was to evaluate the shear bond strengths between various hybrid computer-aided design (CAD)/computer-aided manufacturing (CAM) restorative materials and repairing resin. Two resin network-based hybrid (Lava Ultimate and Polyglass), one ceramic framework-based hybrid (Enamic), and one zirconia (Zenotec Zr bridge) CAD/CAM restorative materials were used in this study. The shear bond strength test and failure modes of four experimental groups designated LUS (Lava Ultimate), ENA (Enamic), PGB (Polyglass), and ZBR (zirconia control group) were characterized in this study. The hybrid CAD/CAM restorative materials showed stronger shear bond strengths in the sequence of PGB, LUS, and ENA (P<0.05). The shear bond strengths of PGB and LUS groups showed significantly higher than those of ZBR (P<0.05), while ENA did not show any significant difference from ZBR (P<0.05). The PEG and LUS groups mostly exhibited cohesive failure, but the ENA and ZBR groups predominantly showed adhesive failure. Therefore, resin network-based hybrid CAD/CAM restorative materials such as Lava Ultimate and Polyglass should be more useful for intra-oral repairs.
초록
본 연구의 목적은 다양한 하이브리드 컴퓨터보조설계(CAD)/컴퓨터보조제작(CAM) 수복재와 수리용 레진 사이의 전단 결합 강도를 평가하는 것이다. 본 연구에서는 2종의 레진 구조 기반 하이브리드(Lava Ultimate 및 Polyglass), 1종의 세라믹 구조 기반 하이브리드(Enamic) 및 1종의 지르코니아(Zenotec Zr brdige) CAD/CAM 수복재를 사용하였고, LUS (Lava Ultimate), ENA (Enamic), PGB (Polyglass), 및 ZBR(지르코니아 대조군)로 각각 명명된 4 개의 실험군의 전단결합강도 및 파절 유형이 평가되었다. 하이브리드 CAD / CAM 수복물은 PGB, LUS 및 ENA 실험군 순서에서 강한 전단 결합 강도를 보였다 (P<0.05). 또한, PGB와 LUS 실험군의 전단 결합 강도는 ZBR 군보다 유의하게 높았으며 (P<0.05), ENA과 ZBR 실험군 간의 전단 결합 강도는 유의한 차이가 없었다 (P<0.05). PEG 및 LUS 실험군은 대부분 응집파절을 나타내었으나, ENA 및 ZBR 실험군은 주로 접착파절을 나타내었다. 따라서 본 연구결과를 토대로 Lava Ultimate 및 Polyglass와 같은 레진 네트워크 기반의 하이브리드 CAD/CAM 수복재가 구강 내 수리에 더 유용하다는 것을 알 수 있었다.
Keywords:
Hybrid CAD/CAM restorative materials, Repairing Resin, Zirconia, Shear bond strength, Intra-oral repair키워드:
하이브리드 CAD/CAM 수복재, 수리용 레진, 지르코니아, 전단결합강도, 구강내 수리INTRODUCTION
Recently, with aesthetic demands and an increase of the patients who want a quick prosthetic treatment and due to the continuous development and popularization of dental computer-aided design (CAD)/computer-aided manufacturing (CAM) equipment, a variety of materials has been developed (Awada & Nathanson, 2015). Most of CAD/CAM restorative materials are variously made of ceramics, composite resins, and acrylic resins (Giordano, 2006), and the composite resins have been widely used since its introduction due to the easy handling and routing processes (O’Brien, 2008). Such composite resins have been developed as the hybrid CAD/CAM restorative materials applied with the latest nanocomposite theory, which are the alternatives to ceramic hybrid CAD/CAM restorative materials (Acar, Yilmaz, Altintas, Chandrasekaran, & Johnston, 2016). The hybrid CAD/CAM restorative materials have different structures, new form of polymerization and innovative microstructure compared to conventional CAD/CAM restorative materials (Mainjot, Dupont, Oudkerk, Dewael, & Sadoun, 2016). They are composed of zirconia-silica nanofillers (80%) including 20 nm diameter zirconia and 4-11 nm diameter silica nanoparticles and resin matrix (20%) in dispersed or aggregated particles forms (Belli, Geinzer, Muschweck, Petschelt, & Lohbauer, 2014b). They have features that provide stability of ceramic network and elasticity of polymer network in a structure that has permeated a secondarily polymerized mixture of Urethane Dimethacrylate (UDMA) and Triethylene Glycol Dimethacrylate (TEGDMA) into the pre-sintered inorganic ceramic (86wt%) support structures (Della Bona, Corazza, & Zhang, 2014). These features exhibit a significant difference from other restorative materials in terms of exposure compared to the ceramic materials, in terms of mechanical and biological properties, chemical stability, adhesion, and long-term viability (Coldea, Swain, & Thiel, 2013; Nguyen, Ruse, Phan, & Sadoun, 2014; Swain, Coldea, Bilkhair, & Guess, 2016).
The hybrid CAD/CAM restorative material is a CAD/CAM material, which has combined the advantages of the ceramic and the resin. It has the advantages of aesthetics similar to the natural tooth, the possible representation of different shades, less abrasion against antagonistic teeth with excellent elasticity, high strength and excellent resistance to discoloration as well as precise reproducibility of margin (Acar et al., 2016; Awada & Nathanson, 2015). It also has other advantages such as a short milling time, a longer life of burs and presentation of better workability compared with the ceramic (Lebon, Tapie, Vennat, & Mawussi, 2015) and the fast production as having no separate sintering step for stain and crystallization. Also, the fact that intra-oral repair can be done simply by using the composite resin would be referred as the biggest difference compared to the conventional ceramic (Zhi, Bortolotto, & Krejci, 2016).
The intra-oral repair is advantageous as it allows a quick treatment in a low-cost, depending on the location and range of fractures (Seabra, Arantes-Oliveira, & Portugal, 2014), and extends the life of fractured prosthesis (Attia, 2010; Raposo et al., 2009). In general, the ceramic has a vulnerability in fracture (Blum et al., 2012), and has been reported with factors to cause fracture such as the defect of ceramic itself, trauma or bad habits (Ozcan & Niedermeier, 2002). In addition to the fracture, there are frequent occurrences of cases that require repairs, such as low occlusion of the prosthesis or the loss of contact points to adjacent teeth, therefore the easiness of repair should be considered when selecting the ceramic materials. In particular, in the case of osseointegrated implants, the interproximal contact surface between the natural teeth and the implant prosthesis tends to be slightly loosened clinically (Kim, Bae, Shim, & Lee, 2005; Wei, Tomotake, Nagao, & Ichikawa, 2008). While an osseointegrated implant to a position where periodontal ligament does not exist, shows immobilization due to the tight adhesion of the bone and very little variation when heavy occlusal force is applied, the natural teeth show the physiological movement due to the presence of periodontal ligament, and acquire the shock-absorbing buffering effect in comparison (Morikawa, 2003; Skalak, 1983). Therefore, there is a need to consider about clinical solutions for the loss of contact points between the implant prosthesis and the adjacent teeth due to the movement of natural tooth after a prosthetic implant treatment.
At present, since there is a shortage of literatures for the clinical effects of intraoral repairs and there is a variety of factors that may affect the bond strength of ceramic and resin for repair, it has still not been defined that the intraoral repairs are efficient to indicate a satisfactory clinical results (Blum et al., 2012; Hickel, Brushaver, & Ilie, 2013). Re-fabrication of a prosthesis is a complete solution, nevertheless, when considered the time and cost-rising factors that may occur in patients due to such re- fabrication, the intraoral repairs within the clinically acceptable range can be an alternative (Hickel et al., 2013; Mohamed, Finkelman, Zandparsa, Hirayama, & Kugel, 2014).
Therefore, this study was conducted with intention to evaluate the shear bond strength of repairing composite resins which was formed according to the hybrid CAD/CAM restorative material, because hybrid CAD/CAM restorative material can be very useful clinically as it makes the intraoral repairs easy and since there was very little data of comparative evaluation on it in previous studies. The objectives of this study were to compare and evaluate the shear bond strength between three kinds of hybrid CAD/CAM restorative materials and the composite resins for repairs recommended by each manufacturer, and to observe the fracture types of them.
MATERIALS AND METHODS
1. Preparation of CAD/CAM restorative material specimen
Lava ultimate (3M ESPE, Seefeld, Germany), Enamic (VITA Zahnfabrick, Bad Säckingen, Germany) and Polyglass (Vericom Co., Korea) were used as the hybrid CAD/CAM restorative materials for this study. Zenotec zr bridge (WielandDental+Technic GmbH, Germany) was used as the zirconia control group (Table 1).
A total of 65 zirconia specimens for each 13 specimens by each group were prepared in disk-shape with size in 12 mm diameter and 3 mm height by using a dental CAD/CAM milling machine (ARUM 5X-200, Doowon Co., Korea). Given the roughness and the precision of the cutting surface due to consumption of bur, a new bur was applied for each group. Zirconia control specimens were sintered 1500℃ for 10 hrs by using Trione-F sintering furnace (DIO Iimplant Co., Korea). The abbreviation of four groups are as follows;
- (1) LUS: Lava ultimate repair kit (3M ESPE, USA) was used.
- (2) ENA: Porcelain repair kit (Ultradent products Inc., South Jordan, UT, USA) and VMLC flow resin (VITA Zahnfabrick, Bad Säckingen, Germany) were used.
- (3) PGB: Polyglass repair kit (Vericom Co., Korea) was used.
- (4) ZBR: Zirconia repair kit (Bredent, Germany) was used.
Also, the detailed information of each group including repair kit and repairing composite resin was listed in Table 2.
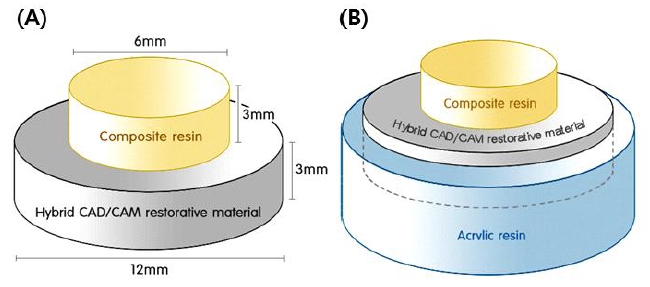
2. Surface treatment for specimens and bonding of repairing composite resins
Aluminum oxide powder (110 ㎛) was sprayed from 10 mm distance vertically with the pressure of 2 bars for 14 seconds to hybrid CAD/CAM and zirconia specimens as described by previous research (Su et al, 2015). Hybrid CAD/CAM specimen was dried after washing by an ultrasonic washing machine for 10 minutes with distilled water to remove residues. Zirconia specimen were cleaned by using compressed air to remove zirconia residues. Bonding procedure of repairing composite resin to CAD/CAM specimen was performed according to the manufacturer's instructions. Bonded specimen was fabricated by using a duralumin mold (6 mm diameter, 3 mm height) as shown in Figure 1. The repairing composite resin was light polymerized by using dental curing light device (Dr's Light Clever Dual, Good Doctors Co., Korea; 1700 mW/cm2 of intensity, 40 seconds of light curing). After the polymerization was completed, the experimental specimen was embedded in acrylic resin to secure it to a jig of a universal testing machine (Figure 2). The specimen was stored at room temperature for 48 hrs, and then the shear bonding strength was performed at room temperature.
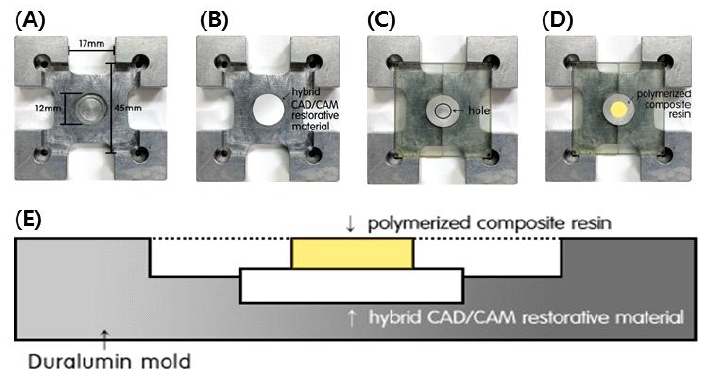
The bonding procedure between CAD/CAM specimens and composite resin. (A) The mold fixing CAD/CAM specimen, (B) Image of locating CAD/CAM specimen onto the center hole of mold, (C) Image of putting mounting bracket to form pellet shaped composite resin, (D) Image of photo-curd composite resin, (E) Schematic diagram of bonding specimen fabrication mold set (Vertical view).
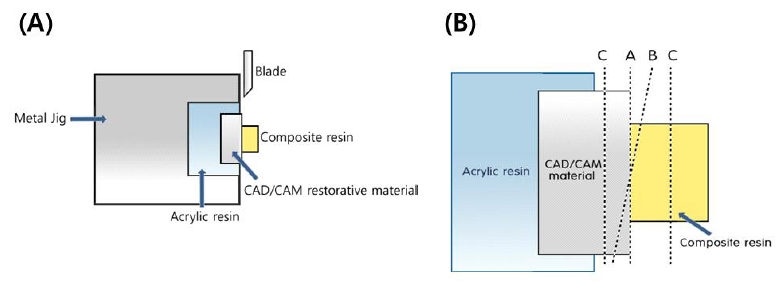
3. Measurement of shear bond strength and analysis of failure modes
A universal testing machine (Z020, Zwick, Germany) was used to measure shear bonding strength. The specimen was secured to a metal jig to ensure the load to be delivered in the same direction to the bonding surface of the specimen and the repairing composite resin and increased the load up to a crosshead speed of 1 mm/min. The maximum load was measured until the repairing composite resin is debonded from the specimen and the shear bonding strength was measured by dividing the adhesive surface with cross-sectional area.
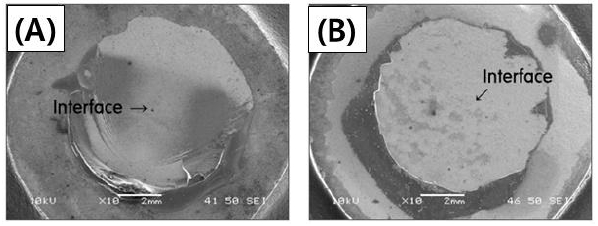
Sixty-five specimens that had incidence of fractures were observed by using a magnifier (8X) and a scanning electron microscope (SEM; JSM-6360, JEOL, Japan) The classification of failure mode after shear bond strength test was described in Figure 3.
4. Statistical Analysis
All data were expressed as means ± standard deviations. The data for shear bond strength test were analyzed statistically by one-way analysis of variance (SPSS 20.0; IBM SPSS, USA) and post-hoc Tukey HSD test. Differences were considered significant if p values were less than 0.05.
RESULTS
1. Shear bond strength test
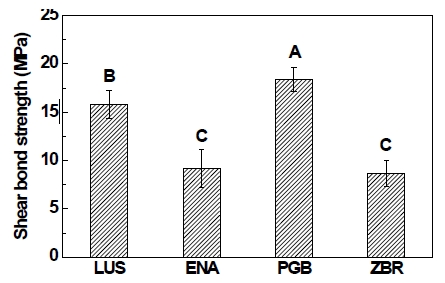
When tested the shear bond strength of hybrid CAD/CAM restorative material and repair composite resin, the shear bond strength value of the PGB group was significantly higher than those of the other groups (P<0.05), and the value of the LUS group was significantly higher than those of the ENA and ZBR group as shown in Figure 4 (P<0.05).
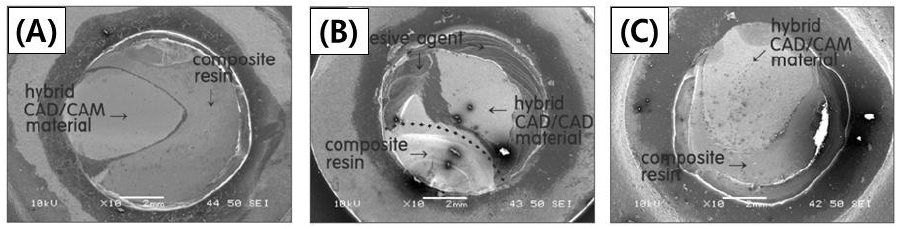
2. Failure modes
Of thirteen specimens in each group, the LUS (Lava Ultimate) and PGB (Polyglass) groups mostly exhibited cohesive failures but no adhesive failure. The ENA (Enamic) group predominantly showed adhesive failures, whereas all specimens of the ZBR (Zirconia) group showed adhesive failures (Table 3). SEM images of cohesive, mixed, and adhesive failure modes were shown in Figure 5, 6, and 7, respectively.
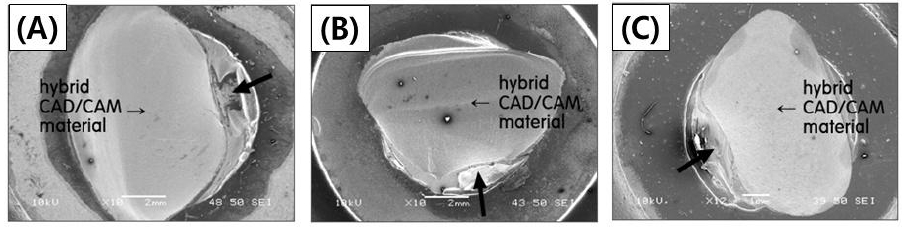
SEM images of cohesive failure mode (A: LUS, B: ENA, C: PGB).* Black arrow indicates load direction.
As a result of observing cohesive fracture sites appeared in hybrid CAD/CAM restorative materials, the mode of failure was in a form of gradual widening according to the loading direction of the force, and as a result of observing mixed fracture sites, hybrid CAD/CAM restorative material and composite resin showed the same mode of failure in the LUS, ENA, and PGB groups. On contrary, when observed the interfaces of the ENA group and the ZBR group that showed adhesive failures, composite resins were clearly separated.
DISCUSSION
From all results of this study, the hybrid CAD/CAM restorative materials showed stronger shear bond strengths in the sequence of the PEG (polyglass), LUS (Lava ultimate), and ENA (Enamic) groups. Additionally, the PEG and LUS groups showed significantly higher shear bond strengths than those of the ZBR group, while the ENA group did not show any significant difference from the ZBR group. This result can be indicated in the structural differences of the hybrid CAD/CAM restorative materials. In terms of the features of each hybrid CAD/CAM restorative material used in the study, Lava ultimate is referred to as Resin Nano Ceramic (RNC) within the scope of the resin composites in the Materials (Elsaka, 2014). They are composed of zirconia-silica nanofillers (80%) and resin matrix (20%) in dispersed or aggregated particles forms, while the ceramics are composed of 20 nm diameter silica and 4~11 nm diameter zirconia nanoparticles (Belli, Geinzer, Muschweck, Petschelt, & Lohbauer, 2014a). Also, Polyglass composed of a ceramic filler (~80%) and the matrix resin (~20%) has structural features like Lava ultimate, and the manufacturer provides hybrid ceramic filler as restorative materials by adopting a curing method which can secure the maximum degree of polymerization in a resin matrix, taking advantage of the technology for high density and high dispersion. Thus, these two hybrid CAD/CAM restorative materials are based on resin-based network structure.
On contrary, Enamic is referred to as polymer-infiltrated ceramic-network material (PICN) and also named as double network materials, ceramic-based interpenetrating phase materials or interpenetrating ceramic-resin composites (Denry & Kelly, 2014; Gracis, Thompson, Ferencz, Silva, & Bonfante, 2015). They have features that provide stability of ceramic network and elasticity of polymer network in a structure that has permeated a secondarily polymerized mixture of UDMA and TEGDMA into the pre-sintered inorganic ceramic (86wt%) support structures (Della Bona et al., 2014). Ceramic network constitutes a three-dimensional support structure that is connected to one another, which disperses the stress more effectively to all directions and represents a structure that can improve the fracture resistance (Swain et al., 2016).
Therefore, the inter-connected support structures of hybrid CAD/CAM restorative materials are divided into a resin network-based and a ceramic framework-based resin in this study. The resin network-based Lava ultimate and Polyglass showed more excellent shear bond strengths to the repairing composite resin than the ceramic network-based Enamic. Resin based repairing materials have been used widely for repairing implant prosthesis prepared by CAD/CAM restorative materials. So, it is no wonder that resin network-based hybrid CAD/CAM restorative prosthesis can be chemically bonded to repairing resin due to similar chemical structure. On contrary, ceramic framework-based hybrid CAD/CAM restorative materials is seemed to be bonded weakly to repairing resin without intermediate coating material such as silane coupling agent because ceramic can only be bonded to resin via physical-mechanical bonding. Therefore, it is clear that resin network-based hybrid CAD/CAM restorative materials are strongly bonded to repairing resin compared to ceramic framework-based CAD/CAM restorative materials are.
Within the limitation of this study, the support structures of hybrid CAD/CAM restorative materials are divided into resin network-based structures and ceramic network-based structures, and it was confirmed that the resin network-based Lava ultimate and Polyglass showed more excellent shear bond strengths to the repairing composite resins than the ceramic network-based Enamic. When the shear bond strength is 10MPa or higher, the material can be used in clinical setting. Among three hybrid CAD/CAM restorative materials such as Lava ultimate, Enamic and Polyglass, Polyglass showed the shear bond strength 2 times higher than zirconia and it was proven with the most excellent outcomes in repairs. Therefore, it is expected that resin network-based hybrid CAD/CAM restorative materials would be more useful for intra-oral repairs compared to ceramic framework-based hybrid CAD/CAM restorative materials are.
CONCLUSION
In this study, the shear bond strengths of three hybrid CAD/CAM restorative materials and repairing composite resins recommended by each manufacturer had been compared and evaluated. Also, it had examined on the outcomes had been shown in comparison to zirconia mainly used as an all-ceramic system in terms of repair and following results had been obtained.
- 1. The hybrid CAD/CAM restorative materials showed stronger shear bond strengths in the sequence of PGB, LUS, and ENA (P<0.05). The shear bond strengths of PGB and LUS groups showed significantly higher than those of ZBR (P<0.05), while ENA did not show any significant difference from ZBR (P<0.05).
- 2. The PEG and LUS groups mostly exhibited cohesive failure, but the ENA and ZBR groups predominantly showed adhesive failure from the results of failure mode observation.
Therefore, resin network-based hybrid CAD/CAM restorative materials such as Lava Ultimate and Polyglass is expected to be more useful for intra-oral repairs.
Acknowledgments
* This paper was supported by Wonkwang university in 2017.
References
-
Acar, O, Yilmaz, B, Altintas, SH, Chandrasekaran, I, Johnston, WM, (2016), Color stainability of CAD/CAM and nanocomposite resin materials, J Prosthet Dent, 115(1), p71-75.
[https://doi.org/10.1016/j.prosdent.2015.06.014]

-
Attia, A, (2010), Influence of surface treatment and cyclic loading on the durability of repaired all-ceramic crowns, J Appl Oral Sci, 18(2), p194-200.
[https://doi.org/10.1590/s1678-77572010000200015]

-
Awada, A, Nathanson, D, (2015), Mechanical properties of resin-ceramic CAD/CAM restorative materials, J Prosthet Dent, 114(4), p587-593.
[https://doi.org/10.1016/j.prosdent.2015.04.016]

-
Belli, R, Geinzer, E, Muschweck, A, Petschelt, A, Lohbauer, U, (2014a), Mechanical fatigue degradation of ceramics versus resin composites for dental restorations, Dent Mater, 30(4), p424-432.
[https://doi.org/10.1016/j.dental.2014.01.003]

- Belli, R, Geinzer, E, Muschweck, A, Petschelt, A, Lohbauer, U, (2014b), Mechanical fatigue degradation of ceramics versus resin composites for dental restorations, Dent Mater, 30(10), p1204-1204.
-
Blum, IR, Nikolinakos, N, Lynch, CD, Wilson, NHF, Millar, BJ, Jagger, DC, (2012), An in vitro comparison of four intra-oral ceramic repair systems, J Dent, 40(11), p906-912.
[https://doi.org/10.1016/j.jdent.2012.07.008]

- Coldea, A, Swain, MV, Thiel, N, (2013), Mechanical properties of polymer-infiltrated-ceramic-network materials, Dent Mater, 29(4), p419-426.
-
Della Bona, A, Corazza, PH, Zhang, Y, (2014), Characterization of a polymer-infiltrated ceramic-network material, Dent Mater, 30(5), p564-569.
[https://doi.org/10.1016/j.dental.2014.02.019]

- Denry, I, Kelly, JR, (2014), Emerging Ceramic-based Materials for Dentistry, J Dent Res, 93(12), p1235-1242.
- Elsaka, SE, (2014), Bond Strength of Novel CAD/CAM Restorative Materials to Self-Adhesive Resin Cement: The Effect of Surface Treatments, J Adhes Dent, 16(6), p531-540.
- Giordano, R, (2006), Materials for chairside CAD/CAM-produced restorations, J Am Dent Assoc, 137, p14s-21s.
-
Gracis, S, Thompson, VP, Ferencz, JL, Silva, NR, Bonfante, EA, (2015), A New Classification System for All-Ceramic and Ceramic-like Restorative Materials, Int J Prosthdont, 28(3), p227-235.
[https://doi.org/10.11607/ijp.4244]

-
Hickel, R, Brushaver, K, Ilie, N, (2013), Repair of restorations -Criteria for decision making and clinical recommendations, Dent Mater, 29(1), p28-50.
[https://doi.org/10.1016/j.dental.2012.07.006]

- Kim, BK, Bae, HE, Shim, JS, Lee, KW, (2005), The influence of ceramic surface treatments on the tensile bond strength of composite resin to all-ceramic coping materials, J Prosthet Dent, 94(4), p357-362.
- Lebon, N, Tapie, L, Vennat, E, Mawussi, B, (2015), Influence of CAD/CAM tool and material on tool wear and roughness of dental prostheses after milling, J Prosthet Dent, 114(2), p236-247.
- Mainjot, AK, Dupont, NM, Oudkerk, JC, Dewael, TY, Sadoun, MJ, (2016), From Artisanal to CAD-CAM Blocks: State of the Art of Indirect Composites, J Dent Res, 95(5), p487-495.
-
Mohamed, FF, Finkelman, M, Zandparsa, R, Hirayama, H, Kugel, G, (2014), Effects of Surface Treatments and Cement Types on the Bond Strength of Porcelain-to-Porcelain Repair, Journal of Prosthodont, 23(8), p618-625.
[https://doi.org/10.1111/jopr.12194]

-
Nguyen, JF, Ruse, D, Phan, AC, Sadoun, MJ, (2014), High-temperature-pressure Polymerized Resin-infiltrated Ceramic Networks, J Dent Res, 93(1), p62-67.
[https://doi.org/10.1177/0022034513511972]

- O’Brien, WJ, (2008), Dental materials and their selection, 4th ed., Quintessence Publishing, Chicago.
- Ozcan, M, Niedermeier, W, (2002), Clinical study on the reasons for and location of failures of metal-ceramic restorations and survival of repairs, Int J Prosthodont, 15(3), p299-302.
- Raposo, LHA, Neiva, NA, da Silva, GR, Carlo, HL, da Mota, AS, do Prado, CJ, Soares, CJ, (2009), Ceramic Restoration Repair: Report of Two Cases, J Appl Oral Sci, 17(2), p140-144.
- Seabra, B, Arantes-Oliveira, S, Portugal, J, (2014), Influence of Multimode Universal Adhesives and Zirconia Primer Application Techniques on Zirconia Repair, J Prosthet Dent, 112(2), p182-187.
- Skalak, R, (1983), Biomechanical coonsiderations in osseointegration prostheses, J Prosthet Dent, 49, p843-848.
-
Swain, MV, Coldea, A, Bilkhair, A, Guess, PC, (2016), Interpenetrating network ceramic-resin composite dental restorative materials, Dent Mater, 32(1), p34-42.
[https://doi.org/10.1016/j.dental.2015.09.009]

- Wei, H, Tomotake, Y, Nagao, K, Ichikawa, T, (2008), Implant prostheses and adjacent tooth migration: Preliminary retrospective survey using 3-dimensional occlusal analysis, Int J Prosthodont, 21(4), p302-304.
-
Zhi, L, Bortolotto, T, Krejci, I, (2016), Comparative in vitro wear resistance of CAD/CAM composite resin and ceramic materials, J Prosthet Dent, 115(2), p199-202.
[https://doi.org/10.1016/j.prosdent.2015.07.011]