The effects of deproteinization and primer treatment on microtensile bond strength of self-adhesive resin cement to dentin
Abstract
The purpose of this study was to evaluate the effects of deproteinization and an additional primer treatment on the microtensile bond strength of a newly developed self-adhesive resin cement to dentin. The occlusal dentin of extracted human third molars was randomly divided into four groups according to the surface treatment: a control (CON) with no treatment; applying a deproteinizing agent (DPT) (5% sodium hypochlorite); using a primer (PRI) (G-CEM ONE Adhesive enhancing primer, GC); and applying a deproteinizing agent and a primer (DPT-PRI). Composite resin blocks with a disk shape (diameter, 10 mm; height, 4 mm) were bonded to the treated dentin using a self-adhesive resin cement (G-CEM ONE, GC). The specimens were sectioned into sticks with a cross-section of 1 mm2 and tested to failure in tension mode at a crosshead speed of 1 mm/min. All groups showed a significantly higher microtensile bond strength compared to CON (p<0.05). PRI showed the highest microtensile bond strength followed by DPT and DPT-PRI (p<0.05). No significant differences were observed between DPT and DPT-PRI (p>0.05). Within the limitations of this study, a deproteinizing agent or specific primer can enhance the microtensile bond strength of the self-adhesive resin cement to dentin. However, it is not recommended to use a primer in combination with the deproteinizing agents.
초록
본 연구의 목적은 탈단백(deproteinization)이나 추가적인 프라이머의 처리가 상아질과 자가접착형 레진 시멘트 사이의 미세인장결합강도에 미치는 영향을 평가하기 위함이다. 총 40개의 사람 제 3 대구치를 선별하여 아크릴 레진에 매몰한 후 교합면의 상아질을 노출시켰다. 표면을 600번 실리콘 카바이드 연마지로 연마하여 도말층을 형성한 후 노출된 상아질에 다음과 같이 처리하였다: 아무런 처리하지않은 대조군; 탈단백제(5% 차아염소산나트륨) 처리; 프라이머(G-CEM ONE Adhesive enhancing primer, GC) 도포; 탈단백제 처리후 프라이머 도포. 복합레진(Filtek Z250, 3M ESPE)을 지름 10 mm, 높이 4 mm의 원통형 플라스틱 주형에 2 mm씩 적층 충전 및 광중합한 후 표면 처리된 상아질에 자가접착형 레진 시멘트(G-CEM ONE, GC)를 적용하고 광중합하여 접착시킨다. 그 후 37℃증류수에 24시간 보관하고 단면이 1 mm2인 막대기 형태로 절단하여 미세인장결합강도를 측정하였다. 각 결과값은 one-way analysis of variance와 Tukey’s honestly significant difference test로 분석하였다. 실험 결과 상아질에 표면 처리를 한 그룹이 대조군에 비해 유의하게 높은 미세인장결합강도를 보였다(p<0.05). 상아질에 프라이머를 단독 처리한 그룹에서 가장 높은 미세인장결합강도가 관찰되었다(p<0.05). 탈단백제 처리나 탈단백제 처리 후 프라이머를 처리한 그룹은 그 다음으로 유의하게 높은 미세인장결합강도를 나타냈으며(p<0.05) 두 그룹 사이에 유의한 차이는 관찰되지 않았다(p>0.05). 결론적으로, 본 연구에 사용한 자가접착형 레진 시멘트는 상아질에 탈단백제나 특정 프라이머를 함께 사용하는 경우 접착력이 향상될 수 있으나 두 제제를 병용하는 것은 추천되지 않는다.
Keywords:
Self-adhesive resin cements, Microtensile bond strength, Deproteinization, Sodium hypochlorite키워드:
자가접착형 레진 시멘트, 미세인장결합강도, 탈단백, 차아염소산나트륨Introduction
With the aim of cementing indirect tooth-colored restorations, resin-based cements have been developed by various dental material manufacturers. These resin-based cements provide numerous advantages such as aesthetics, mechanical strength, low solubility, and bonding ability to enamel and dentin (1). As composite resin-based material, resin cements require pretreatment steps on the tooth substrate. Depending on the adhesive protocol, resin cement has been divided into three groups: total-etch (etch-and-rinse) adhesive resin cement, self-etch (etch-and-dry) adhesive resin cement, and self-adhesive resin cement (2).
The first self-adhesive resin cements (e.g., RelyX Unicem, 3M ESPE, St. Paul, MN, USA) were introduced in 2002. Unlike other resin cements, self-adhesive resin cements do not require any pretreatment of the tooth surface. Simplified adhesive procedures of self-adhesive resin cements might be able to reduce both the sensitivity of the technique and the postoperative sensitivity. According to the manufacturer, self-adhesive resin cements have been claimed to offer several advantages analogous to conventional resin cements (2). Nevertheless, a self-adhesive resin cement is unable to penetrate and/or dissolve the smear layer as in other types of resin cements. Several researchers have shown a superficial interaction between self-adhesive resin cement and dentin with little formation of a hybrid layer and resin tags (3, 4). A recently developed dental material is a new self-adhesive resin cement called G-CEM ONE (GC, Tokyo, Japan), which comes with an additional agent (G-CEM ONE Adhesive enhancing primer, GC, Tokyo, Japan). This agent contains a polymerization initiator and acidic monomers such as 4-{[2-(methacryloyloxy)ethoxy]carbonyl}phthalic acid (4-MET) and 10-methacryloyloxydecyl dihydrogen phosphate (10-MDP), and thus the chemical polymerization of the cement and its penetration into the dentinal tubules can be improved (5-7).
Owing to a substantial loss of tooth structure, dentin has become the main substrate for adhesion through an indirect procedure. However, dentin contains a considerable amount of water, organic components (particularly collagens), and a smear layer that makes it an unfavorable substrate for bonding (3). In this aspect, some researchers have recommended dissolving the collagens with a deproteinizing agent as a way to enhance the bond strength when applied to dentin (8-12). A sodium hypochlorite (NaOCl) solution is a widely used deproteinizing agent that removes organic substances non-specifically from dentin (13). Previous studies have pointed out that an increased mineral-to-matrix ratio of dentin, resembling the composition of mineralized or hypermineralized dentin, through NaOCl treatment, can positively affect the bonding performance of a resin cement (3, 14).
The purpose of this study was to evaluate the effects of deproteinization and an additional primer treatment on the microtensile bond strength of a newly developed self-adhesive resin cement to dentin.
Materials and Methods
1. Specimen preparation
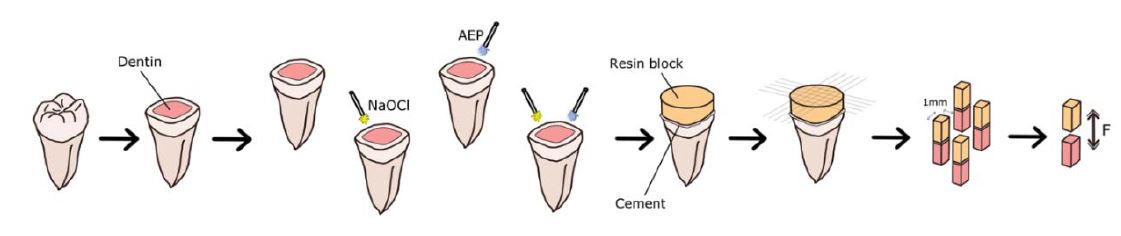
Forty non-carious and non-restored human third molars were used in this study according to the protocol approved by the Institutional Review Board of Pusan National University Dental Hospital (IRB, PNUDH-2018-029). The teeth were stored in a 0.1% thymol solution at 4℃ and used within 1 month after extraction. The roots were embedded at the cervical level in a self-curing acrylic resin (Tokuso Curefast, Tokuyama, Tokyo, Japan) inside plastic blocks to facilitate manipulation. For dentin exposure, the occlusal enamel was ground perpendicular to the long axis of the tooth using a water-cooled high-speed diamond saw (Accutom-50, Struers, Ballerup, Denmark). To obtain a standardized smear layer, the teeth were polished using 600-grit silicon carbide sandpaper under constant water cooling for 1 min. After grinding, the teeth were divided according to the treatment protocol of the dentin. Composite resin disks were made by incrementally building a 2-mm-thick composite resin (Filtek Z250, 3M ESPE, St. Paul, MN, USA) into a cylindrical plastic mold (10 mm in diameter, 4 mm in height), and each increment was polymerized for 40 s using an LED light curing unit (BluePhase G2, Ivoclar Vivadent Inc., Amherst, NY, USA). The sample preparation is shown in Figure 1.
2. Experiment design and bonding procedures
Information on the materials used in this study is provided in Table 1. The self-adhesive resin cement used in this study is composed of a resin cement and a unique primer called a G-CEM ONE Adhesive enhancing primer. The specimens were randomly divided into four groups (ten molars each, n=10) with a treated dentin surface as follows:
- Group 1. Control (CON): No treatment
- Group 2. Deproteinization (DPT): Applying 5% NaOCl (Yuhanrox, Yuhanchlorox Co., Hwaseong, Korea) for 60 s
- Group 3. Primer (PRI): Applying a G-CEM ONE Adhesive enhancing primer for 10 s
- Group 4. Deproteinization + primer (DPT-PRI): Applying 5% NaOCl for 60 s and a G-CEM ONE Adhesive enhancing primer for 10 s
In CON, no treatment was applied to the dentine surface. In DPT and DPT-PRI, a 5% NaOCl solution was actively applied with a disposable applicator for 60 s to obtain deproteinized specimens. After treatment with a 5% NaOCl solution, the specimens were rinsed with water for 15 s and blot-dried using absorbent paper. In PRI and DPT-PRI, a G-CEM ONE Adhesive enhancing primer was applied according to the manufacturer’s instruction. In DPT-PRI, deproteinization was conducted before the primer application. Composite resin blocks were bonded to the dentin specimens using G-CEM ONE cement. The specimens were stored in distilled water at 37℃ for 24 h. The specimens were sectioned into sticks with a cross-section of 1 mm2.
3. Microtensile bond strength (μTBS)
Stick-shaped specimens were fixed to a jig of a tensile testing machine (Micro Tensile tester, Bisco, Schaumburg, IL, USA) using cyanoacrylate glue (Loctite 454, Henkel, Düsseldorf, Germany). The μTBS of the specimens was calculated in MPa and determined under tension at a crosshead speed of 1 mm/min.
4. Failure mode analysis
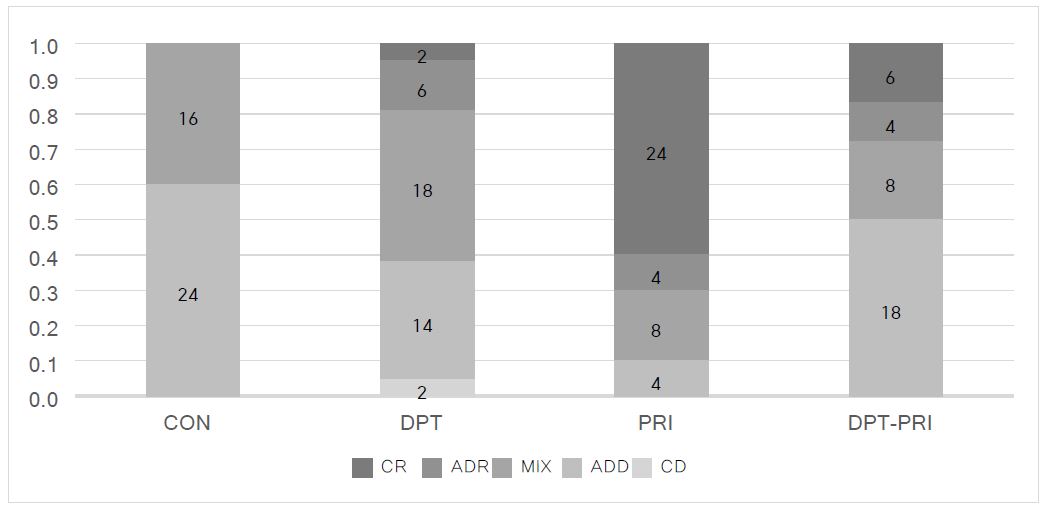
All tested specimens were observed under a stereomicroscope at 40× magnification (Leica, Heidelberg, Germany) to determine the failure mode according to a previously established protocol (15). The failure modes were classified as cohesive in dentin (CD), adhesive between resin cement and dentin (ADD), mixed (MIX), adhesive between resin cement and composite resin (ADR), cohesive in composite resin (CR).
5. Statistical analysis
A statistical analysis was conducted on the mean bond strength of all specimens from each group. A one-way analysis of variance (ANOVA) and Tukey’s honestly significant difference test were applied to determine any statistical differences between groups using SPSS 21.0 software (SPSS Inc., Chicago, IL, USA) at a significance level of p=0.05.
Results
A one-way ANOVA showed a significant effect of deproteinization or additional primer on the bond strength of a self-adhesive resin cement (G-CEM ONE) to dentin (p<0.05).
The mean and standard deviations of the microtensile bond strength data of the tested groups are shown in Table 2. PRI showed the highest mean bond strength values, followed by DPT and DPT-PRI (p<0.05). No significant differences in the microtensile bond strength were observed between DPT and DPT-PRI (p>0.05). In addition, CON showed the lowest microtensile bond strength among all groups (p<0.05).

Mean and standard deviation (SD) of microtensile bond strength (MPa) obtained in each dentinal treatment(n=10)
Figure 2 shows the distribution of failure modes within groups. In CON, the failure mode was predominantly adhesive, followed by a mixed failure. In DPT and DPT-PRI, adhesive and mixed failures were frequently observed. Among all groups, a cohesive failure in dentin was observed solely in DPT. The most frequent failure mode in PRI was a cohesive failure in the composite resin.
Discussion
Based on the results of the microtensile bond strength test reported in the current study, it can be concluded that deproteinization or an additional primer can enhance the bond strength of a self-adhesive resin cement to dentin. In addition, no significant difference was observed between the DPT and deproteinization group in combination with an additional primer treatment (DPTPRI).
Deproteinization has been proven to be effective in enhancing the bond strength of the tooth substrate and the restorative materials. NaOCl is a frequently used and effective deproteinizing agent (16). In similar studies, deproteinized surfaces showed extensive porosity with widened openings of the dentinal tubules and exposed holes in the inter-tubular dentin (lateral ramifications) that increase the permeability (8, 17-20). Moreover, previous studies have shown that NaOCl partially dissolves the organic components of the smear layer, thinning the layer (14, 21). This smear layer with less disorganized collagen and a gelatinous layer may enhance the bonding performance of a self-etch adhesive.
Compared to other studies, the deproteinized dentin group (DPT, DPT-PRI) considered in the present study showed a significantly higher microtensile bond strength compared to CON. The improved bond strength values are also associated with the chemical mechanisms of the deproteinization process. Through this process, numerous hydroxyapatite crystals that can interact with adhesive monomers were exposed (22). The self-adhesive resin cement and additional primer used in this study include a functional monomer called 10-MDP, which reacts chemically with hydroxyapatite crystals and forms 10-MDP-Ca salts. This chemical bond may also be related to the improved bond strength of DPT compared to that of CON.
By contrast, a previous study showed that exposure to a deproteinizing agent significantly impairs the bonding of an adhesive agent to dentin (23). In addition, a systematic review regarding the effect of deproteinization on the bonding of a self-etch adhesive to dentin showed that a lengthy exposure to the deproteinizing agent adversely affects the bonding to dentin (24). This may be attributed to the oxidization effect of the NaOCl solution. Several investigators have speculated that the super-oxide radicals formed through the NaOCl interrupt the propagation stage during the polymerization of the resin monomers (4, 25). Nonetheless, in this study, higher bond strength values were observed in DPT as compared to CON. The increased permeability of dentin, partial dissolution of the smear layer, and the interaction between adhesive monomers and hydroxyapatite crystals possibly compensate for the bond strength, which may be hampered by the oxidization stress.
The chemical compositions of the self-adhesive resin cement used and its additional primer are not specifically known. According to the manufacturer, the primer (G-CEM ONE Adhesive enhancing primer) contains methacrylate monomers such as 4-MET and 10-MDP. These acidic functional monomers increase the infiltration of resin monomer into the dentin. Thus, the superficiality of a self-adhesive resin cement may be improved to form a thicker hybrid layer. In addition, the manufacturer claims that “touch curing” occurs on the interface of the cement (G-CEM ONE) and its primer including a polymerization initiator. This may explain the highest microtensile bond strength of PRI among all groups.
Although the deproteinization and primer treatment increased the bond strength of the self-adhesive resin cement to dentin, an additive effect was not shown in DPT-PRI. When organic components were dissolved using a NaOCl solution, an increase in the mineral content and a reduction in water content occur. A previous study mentioned that a reduced water content might be advantageous for a hydrophobic self-adhesive resin cement to improve the surface wettability (4). Accordingly, the cements used in this study may infiltrate into dentin treated with a NaOCl solution even more deeply than CON. By contrast, a reduction in the amount of water might have an adverse effect on the primer. It is well known that water ionizes the acidic groups, allowing the formation of hydronium ions (H3O+), which demineralize the dentin surface (26). A reduction in the amount of water may be followed by a reduction in the ionization of the acidic monomers of the primer, which may hamper the demineralization action of the acidic moieties. For this reason, it is not recommended to use a deproteinizing agent and the primer all at once when cementing using G-CEM ONE cement.
One noteworthy observation was the failure mode distribution of the DPT. Among all specimens considered, a cohesive failure of dentin was observed only in DPT. The results indicate that a deproteinizing technique may affect the integrity of the dentin. It was reported that NaOCl may deteriorate the mechanical properties of dentin through a degradation of intact organic components (27).
The results of this study indicate that the deproteinization technique is a practical way to achieve an improved bonding performance of a self-adhesive resin cement to dentin without purchasing an additional primer. Nonetheless, further studies are needed to investigate the possible effects of deproteinizing agent on integrity of dentin.
Conclusion
Within the limitations of this study, a deproteinization technique or additional primer (G-CEM ONE Adhesive enhancing primer) treatment was shown to enhance the microtensile bond strength of a self-adhesive resin cement (G-CEM ONE) to dentin. However, the use of a primer in combination with a deproteinizing agent is not recommended.
Acknowledgments
This work was supported by a 2-Year Research Grant of Pusan National University
References
-
Hikita, K, Van-Meerbeek, B, De Munk, J, Ikeda, T, Landuyt, KV, Maida, T, et al. , Bonding effectiveness of adhesive luting agents to enamel and dentin, Dent Mater., (2007), 23(1), p71-80.
[https://doi.org/10.1016/j.dental.2005.12.002]

- Radovic, I, Monticelli, F, Goracci, C, Vulicevic, ZR, Ferrari, M, Self-adhesive resin cements: A literature review, J Adhes Dent., (2008), 10(4), p251-8.
- Barbosa, De, Souza, F, Sinclér Delfina, C, Lacalle Turbino, M, Braz, R, Deproteinized dentin: A favorable substrate to self-bonding resin cements, J Biomed Mater Res B., (2011), 98(2), p387-94.
-
Kambara, K, Nakajima, M, Hosaka, K, Takahashi, M, Thanatvarakorn, O, Ichinose, S, et al. , Effect of smear layer treatment on dentin bond of self-adhesive cements, Dent Mater J., (2012), 31(6), p980-7.
[https://doi.org/10.4012/dmj.2012-031]

-
Giannini, M, Makishi, P, Ayres, AP, Vermelho, PM, Fronza, BM, Nikaido, T, et al. , Self-etch adhesive systems: A literature review, Braz Dent J., (2015), 26(1), p3-10.
[https://doi.org/10.1590/0103-6440201302442]

-
Wang, T, Nikaido, T, Nakabayashi, N, Photocure bonding agent containing phosphoric methacrylate, Dent Mater., (1991), 7(1), p59-62.
[https://doi.org/10.1016/0109-5641(91)90029-x]

-
Chigira, H, Yukitani, W, Hasegawa, T, Manabe, A, Itoh, K, Hayakawa, T, et al. , Self-etching dentin primers containing phenyl-P, J Dent Res., (1994), 73(5), p1088-95.
[https://doi.org/10.1177/00220345940730051101]

-
Pioch, T, Kobaslija, S, Huseinbegovic, A, Müller, K, Dörfer, C, The effect of NaOCl dentin treatment on nanoleakage formation, J Biomed Mater Res., (2001), 56(4), p578-83.
[https://doi.org/10.1002/1097-4636(20010915)56:4<578::aid-jbm1130>3.0.co;2-#]

- De Souza, FB, Silva, CHV, Palma Dibb, RG, Delfino, CS, Beatrice, LCS, Bonding performance of different adhesive systems to deproteinized dentin–microtensile bond strength and scanning electron microscopy, J Biomed Mater Res B., (2005), 75(1), p158-67.
-
Maior, JR, Da Figueira, MA, Netto, AB, de Souza, FB, da Silva, CH, Tredwin, CJ, The importance of dentin collagen fibrils on the marginal sealing of adhesive restorations, Oper Dent., (2007), 32(3), p261-5.
[https://doi.org/10.2341/06-75]

- Erhardt, MCG, Osorio, E, Aguilera, FS, Proenca, JP, Osorio, R, Toledano, M, Influence of dentin acid-etching and NaOCl-treatment on bond strengths of self-etch adhesives, Am J Dent., (2008), 21(1), p44-8.
-
Sauro, S, Mannocci, F, Toledano, M, Osorio, R, Pashley, DH, Watson, TF, EDTA or H3PO4/NaOCl dentine treatments may increase hybrid layers’ resistance to degradation: A microtensile bond strength and confocal-micropermeability study, J Dent., (2009), 37(4), p279-88.
[https://doi.org/10.1016/j.jdent.2008.12.002]

-
Sakae, T, Mishima, H, Kozawa, Y, Changes in bovine dentin mineral with sodium hypochlorite treatment, J Dent Res., (1988), 67(9), p1229-34.
[https://doi.org/10.1177/00220345880670091601]

- Mountouris, G, Silikas, N, Eliades, G, Effect of sodium hypochlorite treatment on the molecular composition and morphology of human coronal dentin, J Adhes Dent., (2004), 6(3), p175-82.
- Kwon, SJ, Park, JK, Son, SA, Shear bond strength between universal adhesives with various pH and dual-cured resin cements, Korean J Dent Mater., (2017), 44(4), p301-10.
-
Hawkins, CL, Davies, MJ, Hypochlorite-induced damage to proteins: formation of nitrogen-centred radicals from lysine residues and their role in protein fragmentation, Biochem J., (1998), 332(3), p617-25.
[https://doi.org/10.1042/bj3320617]

- Wakabayashi, Y, Kondou, Y, Suzuki, K, Yatami, H, Yamashita, A, Effect of dissolution of collagen on adhesion to dentin, Int J Prosthodont., (1994), 7(4), p302-6.
-
Inaba, D, Duschner, H, Jongebloed, W, Odelius, H, Takagi, O, The effects of a sodium hypochlorite treatment on demineralized root dentin, Eur J Oral Sci., (1995), 103(6), p368-74.
[https://doi.org/10.1111/j.1600-0722.1995.tb01859.x]

-
Marshall, GW, Marsall, SJ, Kinney, JH, Balooch, M, The dentin substrate: Structure and properties related to bonding, J Dent., (1997), 25(6), p441-58.
[https://doi.org/10.1016/s0300-5712(96)00065-6]

- Perdigão, J, Thompson, JY, Toledano, M, Osório, R, An ultra-morphological characterization of collagendepleted etched dentin, Am J Dent., (1999), 12(5), p250-5.
- Montes, MA, de Goes, MF, Sinhoreti, MA, The in vitro morphological effects of some current pre-treatments on dentin surface: A SEM evaluation, Oper Dent., (2005), 30(2), p201-12.
-
Augusto, MG, Torres, C, Pucci, CR, Schlueter, N, Borges, AB, Bond stability of a universal adhesive system to eroded/abraded dentin after deproteinization, Oper Dent., (2018), 43(3), p291-300.
[https://doi.org/10.2341/16-173-l]

-
Yamauti, M, Hashimoto, M, Sano, H, Ohno, H, Carvalho, RM, Kaga, M, et al. , Degradation of resin-dentin bonds using NaOCl storage, Dent Mater., (2003), 19(5), p399-405.
[https://doi.org/10.1016/s0109-5641(02)00083-0]

-
Alshaikh, KH, Hamama, HHH, Mahmoud, SH, Effect of smear layer deproteinization on bonding of self-etch adhesives to dentin: A systematic review and meta-analysis, Restor Dent Endod, (2018), 43(2).
[https://doi.org/10.5395/rde.2018.43.e14]

-
Taniguchi, G, Nakajima, M, Hosaka, K, Iwamoto, N, Ikeda, M, Foxton, RM, et al. , Improving the effect of NaOCl pretreatment on bonding to caries-affected dentin using self-etch adhesives, J Dent., (2009), 37(10), p769-75.
[https://doi.org/10.1016/j.jdent.2009.06.005]

- Salz, U, Zimmerman, J, Zeuner, F, Moszner, N, Hydrolytic stability of self-etching adhesive systems, J Adhes Dent., (2005), 7(2), p107-16.
-
Fuentes, V, Toledano, M, Osorio, R, Carvalho, RM, Microhardness of superficial and deep sound human dentin, J Biomed Mater Res A., (2003), 66(4), p850-3.
[https://doi.org/10.1002/jbm.a.10064]