Effect of core surface treatment on the fracture resistance of zirconia restoration
The purpose of this study was to examine the effect of acid-base surface treatment on the fracture resistance, which is one of main mechanical property, of zirconia restoration in order to improve the bonding characterization between zirconia core and ceramic veneer in bi-layered all ceramic restoration system. 10% hydrofluoric acid (HF) and 1 M sodium hydroxide (NaOH) were used as acid and base chemical solutions for surface treatment, respectively. Fracture-resistance tests were performed to investigate the effects of acid and liner treatment on the improvement of the bonding strength between veneer ceramics and zirconia. Specimens were divided into five groups (n = 4) according to the type of surface treatment: (1) Group A, no treatment (control); (2) Group B, liner treatment; (3) Group C, 10% HF etching for 60 s; (4) Group D, 10% HF etching for 60 s and liner treatment. All results of fracture resistance test showed that there were no significant differences between surface treatment types. Failure mode observation indicated that most specimens of Cerasys, Zmatch, and ICE groups showed cohesive failure mode regardless of the method of surface treatment. From the results of study, the short (1 min) treatment of zirconia in HF solution is supposed to be suitable for improving bond strength of zirconia restoration, but long (more than 30 min) treatment of zirconia in HF solution is expected to deteriorate the zirconia structure. Also, several factors such as liner and acid treatment, which improve the fracture resistance of zirconia restoration, seemed to depend on the type of zirconia materials.
Keywords:
bond characterization, fracture resistance, hydrofluoric acid, sodium hydroxide, surface treatment, zirconia restorationINTRODUCTION
Since the development of porcelain fused to metal (PFM) procedures in the early 1960s, metal ceramic restoration has represented the “gold standard” for years in dentistry because of good mechanical properties and a clinically acceptable quality of their marginal and internal adaptation (Zarone et al., 2011). The increasing demand for esthetics, along with biological concerns about some metallic restorations, has stimulated research in metal-free, natural, tooth-colored restorations. All-ceramic restoration has several advantages, including long-term color stability, biocompatibility, and wear resistance (Rosenstiel et al., 2001; Sjogren et al., 2000). However, limited marginal adaptation, excessive wear of the opposing dentition, aggressive preparation design, technique sensitivity, and susceptibility to fracture were the main disadvantages of all-ceramic restorations (Rosenstiel et al., 2001; Blatz, 2002). Generally, fabrication defects such as internal voids, porosities, or microstructural features and surface cracks such as defects on the surface caused by machining and the grinding process compromise the ability of all-ceramic restoration in withstanding occlusal forces (Drummond and Eliades, 2003; Rosenstiel et al., 2001).
Failure of all-ceramic restoration begins with microscaled damage created by the interaction of preexisting defects with applied load forces (Drummond and Eliades, 2003). Failure can also occur by the impact forces or subcritical crack growth enhanced in an aqueous environment (Zahran et al., 2008). In general, dental restorations made by zirconia systems should resist fracture better than other conventional all-ceramic restorations, especially in regions where excessive occlusal loads are anticipated. However, zirconia is not transparent and cannot be stained to expect excellent esthetic results. To improve the esthetic property of zirconia, it must be veneered with suitable porcelain exhibiting high transparency. In all-ceramic systems, the ceramic framework is rigid and does not yield to the stress induced by a thermal mismatch. Therefore, the risk of formation of destructive stress in the veneer layer might be higher in all-ceramic systems and would require a high mechanical strength for veneering materials. Hence, the strength of the veneering ceramic is a crucial parameter for the clinical long-term success of all-ceramic restorations (Fischer et al., 2008).
Unfortunately, this zirconia-porcelain double layer arrangement is expected to increase the complexity of stress distribution within the restoration, resulting in the debonding of zirconia and porcelain and making the prediction of its performance difficult. Zirconia is well known to have a relatively inactive surface because of the lack of surface energy and lower inert property (Wedler, 2004). Therefore, numerous techniques have been introduced to activate the zirconia surface, which has insufficient hydroxyl functional groups at its surface (kern and Wegner 1998; Atsu et al., 2006). Many researches related to zirconia surface treatment have been performed to investigate the effect of amino or hydroxyl acid or base in a variety of time and temperature on the surface structure of zirconia (Uchida al., 2002; Galoppini, 2004: Fischer al., 2005; Touzi al., 2006: Lohbauer al., 2008). Etching the dental ceramic surface with hydrofluoric acid or acidulated phosphate fluoride gel is a common procedure for fabricating a microscaled retentive surface before bonding the ceramic restorations because both acids can etch porcelain and thus create a mechanically retentive surface (Canay et al., 2001). Type and concentration of the etchant and etching duration can influence bond strength of core and veneer (Canay et al., 2001). Therefore, in order to optimize bond strength, acid concentrations and etching durations should be adjusted with respect to specific porcelains (Canay et al., 2001). Tough bioactive materials can be prepared by the chemical treatment of metals and ceramics that have high fracture toughness, e.g., by the NaOH and heat treatments of titanium metal, titanium alloys, and tantalum metal, and by H3PO4 treatment of tetragonal zirconia (Kokubo al., 2004).
Although zirconia shows superior mechanical performance (in terms of strength, toughness, and fatigue resistance) compared to conventional ceramic materials, a consistent problem that one faces while working with zirconia is its poor adhesion to various substrates (synthetic or living such as tissues) encountered in dental or other biomedical applications. Conventional cementation and/or attachment techniques used with zirconia components do not provide sufficient bond strength for many clinical applications because of its inert surface characteristics (Blatz et al., 2002, 2003, 2007).
Feldspar ceramic liner, including selenium, was introduced for the first time from Degudent GmbH; this liner was used to compensate for the white color of zirconia. In addition, this liner has been reported to affect the bond strength of core and veneering ceramic materials. Aboushelib (2005) reported that the use of liner between the core and all-ceramic veneer doubled the bond strength of core and all-ceramic veneer; Aboushelib et al. (2006) reported that adhesive strength was affected by the type of the ceramic and the existence of liner.
This is also the reason why zirconia frameworks show high resistance to strong chemical agents such as acids, alkalis, and organic/inorganic solvents (Blatz et al., 2002). Therefore, high retention, prevention of micro- leakage, and increased fracture and fatigue resistance play an important role in the establishment of a reli- able bonding technique between zirconia and porcelain.
The purpose of the presents study was the zirconia surface is converted to a more reactive zirconia surface with high mechanical retention, enabling improved bonding to other dental substrates. It also shows the combined effect of liners used for enhancing bond characterization of zirconia and chemical treatments on the fracture resistance of zirconia restoration.
MATERIALS AND METHODS
1) Metal die specimen
The main model specimen used in this study was full-crown metal master die (stainless steel, AISI type 303, Korea) with coronal diameter of 7.95 mm, cervical diameter of 9.00 mm, height of 5.00 mm, and 6° taper [Fig. 1(a)].
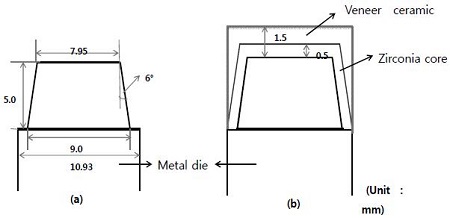
Schematic drawing of specimens used in the study. (a) The metal master die made of stainless steel, (b) All ceramic crown; core and veneer ceramic.
Three core zirconia restorations such as Cerasys ZR (Cerasys, USA), Zmatch (Dentaim, Korea), and ICE Zircon (Zirkonzahn®, Italy) were used as experimental groups for fracture resistance test. Ten specimens were prepared in each group. IPS e.max Ceram (Ivoclar, Liechtenstein) was used for veneer ceramic (Table 1).
2) Zirconia core preparation and surface treatment
Dental ceramic cores are difficult to process if perfectly sintered zirconia is used; therefore, a presintered zirconia block is often employed. Because the contraction caused by the calcination of presintered zirconia reaches up to approximately 21%, it is designed by magnification to complement the amount of contraction achieved with the CAD program and sent to the CAM equipment for mechanical processing. Presintered zirconia blocks were milled according to the manufacturer’s instructions. Then, they were cleaned, dried, and sintered according to the suggested firing schedules (Table 1). After Presintered Y-TZP blocks was milled, the temperature was increased up to 1500 °C or 1600 °C from 20 °C and maintained at that temperature for 2 h in a zirconiasintering furnace to prepare the zirconia core (Table 4).
Forty 0.5 mm thick zirconia core specimens were fabricated in each experimental group [Fig. 1(b)].
Fracture resistance tests were performed to investigate the effects of acid and liner treatment on the improvement of the bond strength between veneering ceramics and sintered zirconia core. Specimens were divided into five groups (n = 4) according to the type of surface treatment: (1) Group A; no treatment (control), (2) Group B; liner treatment, (3) Group C; 10% HF etching for 60 s, (4) Group D; 10% HF etching for 60 s and liner treatment (Table 2).
Group C and D were etched 10% HF during 60 s. Group B and D was built up to a thickness of 0.1 mm to used IPS e-max Ceram Liner and it was sintered at 960 °C (Table 1).
3) Porcelain build-up
Veneer ceramics were built up by using dentin porcelain. The specimens was applied Dentine with IPS e.max Ceram A3 color, and then they were sintered at 750 °C. Additional dentine ceramic was applied to adjust the dimension of the final product as much as it was shrunk. After that, the glazings of final specimens were made at 725 °C. The final thickness of the occlusal surface including zirconia core and veneering ceramic was adjusted to 1.5 mm [Fig. 1(b)]. The specimens were sintered at the ceramic furnace according to the manufacturer’s instruction (Table 1).
4) Measurement of fracture resistance
Self-adhesive resin cement (Rely-X Unicem, 3M, USA) was used to cement each zirconia core to a metal master die to simulate clinical situations [Fig. 2(a)]. Complete samples were cemented with self- adhesive resin cement, and then load the static load of the compressor were added for 10 s with 2kg. then immersed in distilled water at 37 °C for 24 h. Fracture resistance was loaded on the center occusal by round punch (diameter 4.0 ㎜) at a crosshead speed of 1.0 ㎜/min until failure occurred by the universal testing machine [Fig. 2(b), (c)].
5) Failure mode
Fracture pattern was observed using an SEM (JSM 6360, JEOL, Tokyo, Japan) with 8 magnification. One SEM image per specimen was obtained to determine the type of failure mode of the specimen. The type of failure mode was classified as cohesive, adhesive, and mixed.
6) Statistical analysis
The results of the fracture resistance test were statistically analyzed with one-way ANOVA using the SPSS 12.0 program, followed by Tukey HSDa multiple range test (α = 0.05). The results of the fracture resistance test were statistically analyzed with two-way analysis of variance (ANOVA) by the combinatory effect of liner and acid-surface treatments and materials, followed by Tukey HSDa multiple range test (α = 0.05).
RESULTS
1) Fracture resistance
Fig. 3 shows the results of fracture resistance of zirconia restorations with various surface treatments. The results of the Cerasys group showed there was no significant difference between the surface treatments, even though the value of the liner-treated specimen showed a tendency toward being higher than that of other groups (P>0.05). From the results of Zmatch group, there was no significant difference between the surface treatments, even though the value of liner- and HF-treated specimen showed a tendency toward being higher than that of other groups (P>0.05). The results of the ICE group revealed that the fracture resistance of the non-treated specimen was higher than that of other groups; however, there was no significant difference between the experimental groups (P>0.05). The results of fracture resistance were statistically analyzed by two-way ANOVA to confirm the interaction of materials and treatment type. As shown in Table 3, there was significant interaction between the materials and the treatment types; this interaction was caused by the materials, not by the treatment type (P<0.05).
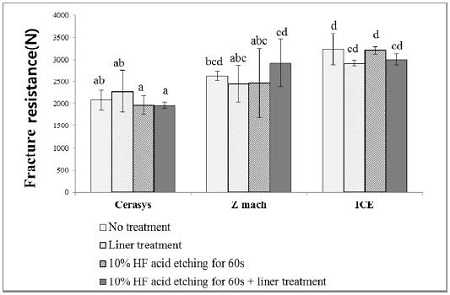
Fracture resistance of all ceramic system. The same letters were not significantly different by two- way ANOVA and Tukey HSDa multiple range test at α=0.05.
2) Failure mode
All specimens were gold coated with a sputter coater (Balzers-SCD 050; Balzers Union, Aktiengesellschaft, Fürstentum, Liechtenstein) for 180 s at 40 mA. The failure mode was obtained from the specimen’s SEM image after performing the fracture-resistance test (Fig. 4). As shown in Table 4, most specimens of all experimental groups had mixed failure modes composed of cohesive failure in the zirconia core and adhesive failure at the interface of the zirconia core and ceramic veneer.
Fail modes classified of fracture described in Fig. 4. (a) cohesive failure in core (b) adhesive failure at the core/veneering interface.
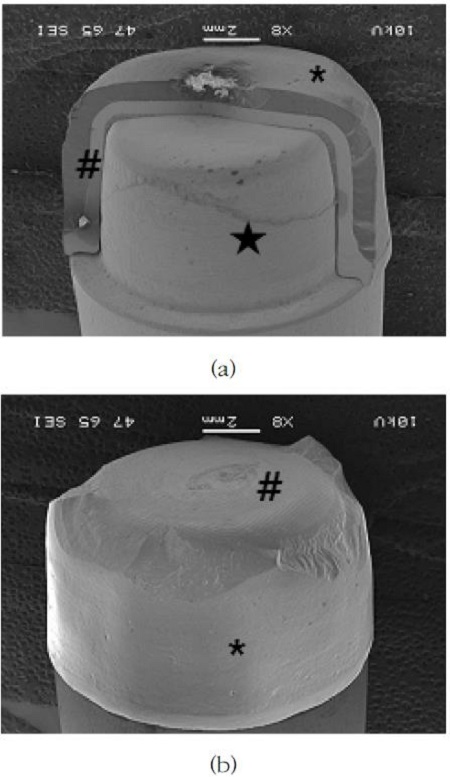
Representative failure images of all ceramic systems by scanning electron microscopic observation at ×8, (a) cohesive failure in core (b) adhesive failure at the core/veneering interface. ( * : veneering ceramic, # : core ceramic, ★ : metal master die)
DISCUSSION
Study mainly confirmed the fracture resistance and failure mode of full-crown shaped zirconia restoration treated by liner and 10% HF. As mentioned before (Jeoung et al., 2012), the duration of 10% HF treatment is determined to be 1 min to optimize the etching condition of HF. It has been reported that the fracture of double-layered all-ceramic restoration is mainly caused by the defect in the fabrication process, occurrence of residual stress because of the mismatch of the thermal expansion coefficient, and structural transformation of zirconia at the interface of core and all-ceramic veneer (Albakry et al., 2003).
In this study, the Cerasys group showed a tendency toward the augmentation of fracture resistance, even though there was no significant difference between the conditions of surface treatment (P>0.05). Z-match and ICE groups did not show any liner-treatment related augmentations. From the results of most of the previous research, the application of liner to zirconia surfaces was one of the main methods to improve the bond strength of zirconia cores with veneered/cemented ceramic. However, Aboushelib (2008) reported the possibility of the development of structural defects, including air bubbles, because of the liner. Swain (2009) also reported that experimental factors related to interfacial stress stem from the mismatch of the thermal contraction of zirconia cores and all-ceramic restorations, which was considered to resolve the interaction and bonding mechanism of zirconia core and all-ceramic veneer. In addition, it is well known that all-ceramic restorations have natural defects generated during the fabrication process; these unpredictable and uncountable defects are supposed to affect the bond strength of the core and all-ceramic veneer and eventually the unwanted fracture of zirconia all-ceramic restoration.
The results of the failure mode after performing fracture-resistance test showed that most specimens of all experimental groups had mixed failure modes composed of cohesive failure in zirconia cores and adhesive failure at the interface of zirconia core and ceramic veneer (Table 4).
The fracture pattern of zirconia all-ceramic restoration generally indicates the pattern of bulk fracture of the core and veneering ceramic fractured at the same time without lamination. Lawn (2004) reported that the radial crack occurs suddenly when a specific load is applied. It propagated toward the specimen exterior when a load was continuously applied. In general, crack tended to remain in the zirconia core so that the zirconia all-ceramic restoration could withstand additional mechanical force. However, when strong load was applied to the restoration, the crack would propagate to the entire restoration area, leading to a huge failure.
In general, specimens with low bond strength showed adhesive failure, and those with high bond strength exhibited cohesive and mixed failure modes, though the failure-mode pattern and the results of bond strength showed poor correlation. Also, previous studies reported that the value of the bond strength of the core and all-ceramic veneer with 3.4–61.0 MPa strength was affected by the testing equipment, type of resin cement, type of veneering ceramic, and surface conditions (Aboushelib et al., 2005).
In this study, the fracture resistance of all experimental groups after surface treatment showed a tendency to decrease mildly. The average magnitude of occlusal forces during chewing or swallowing is known to be 40 N; the maximum magnitude loaded to posterior is variously reported as varying from 200 to 540 N (Strub and Beschnidt, 1998). Therefore, when the results of the fracture-resistance test is compared to the average force applied to natural teeth, surface-treated zirconia all-ceramic restoration tested in this study is supposed to be able to withstand the maximum occlusal forces applied at the posterior teeth.
Many factors affect bond strength, such as the loading speed rate, stress distribution type, thickness ratio, length and width of the combined surface, location of the starting point of fracture, and paths of crack spread. Therefore, the absolute value of the bond strength measured in the laboratory may not be appropriate to interpret as a clinical result. This result seems to be useful for relative comparison and assessment (Denry and Kelly, 2008). The fracture of ceramics is reported to be caused by the fatigue owing to repeated small load rather than large force acting on it temporarily; therefore, the above factors should be further researched.
CONCLUSION
The fracture resistance test of full-crown shaped zirconia all-ceramic specimen were performed to investigate the effect of acid surface treatment on the fracture resistance of zirconia all-ceramic restoration in order to improve the bonding characterization between zirconia core and ceramic veneer in double-layered all-ceramic restoration system and the results of both tests are as follows;
The results of fracture resistance showed that there were no significant differences between surface treatment types, even though there was interaction between materials and the type of surface treatment. Failure mode observation after fracture resistance indicated that most specimens of all experimental groups showed cohesive failure regardless of the method of surface treatment.
From the results of study, several factors such as liner and acid treatment, which seems to improve the fracture resistance of zirconia restoration, seemed to be independent of materials and the type of surface treatment. Therefore, further investigation including more factors affecting the bond strength of zirconia and veneer ceramic is expected to be performed to optimize the condition of bonding technique and understand the bonding mechanism of core and veneer ceramic in clinical situation.
References
-
Aboushelib, MN, de Jager, N, Kleverlaan, CJ, Feilzer, AJ, (2005), Microtensile bond strength of different components of core veneered all-ceramic restorations, Dent Mater, 21(10), p984-991.
[https://doi.org/10.1016/j.dental.2005.03.013]

- Aboushelib, MN, Kleverlaan, CJ, Feilzer, AJ, (2006), Microtensile bond strength of different components of core veneered all-ceramic restorations. Part II: Zirconia veneering ceramics, Dent Mater, 22(9), p857-863.
-
Aboushelib, MN, Matinlinna, JP, Salameh, Z, Ounsi, H, (2008), Innovations in bonding to zirconia based materials: Part I, Dent Mater, 24(9), p1268-1272.
[https://doi.org/10.1016/j.dental.2008.02.010]

- Aboushelib, MN, Aboushelib, MN, Mirmohamadi, H, Matinlinna, JP, Kukk, E, Ounsi, HF, Salameh, Z, (2009), Innovations in bonding to zirconia-based materials. Part II: Focusing on chemical interactions, Dent Mater, 25(8), p989-993.
-
Albakry, M, Guazzato, M, Swain, MV, (2003), Fracture toughness and hardness evaluation of three pressable all-ceramic dental materials, J Dent, 31(3), p181-188.
[https://doi.org/10.1016/S0300-5712(03)00025-3]

-
Atsu, SS, Kilicarslan, MA, Kucukesmen, HC, Aka, PS, (2006), Effect of zirconium-oxide ceramic surface treatments on the bond strength to adhesive resin, J Prosthet Dent, 95(6), p430-436.
[https://doi.org/10.1016/j.prosdent.2006.03.016]

- Blatz, MB, (2002), Long-term clinical success of all-ceramic posterior restorations, Quintessence Int, 33(6), p415-426.
-
Blatz, MB, Sadan, A, Kern, M, (2003), Resin-ceramic bonding: a review of the literature, J Prosthet Dent, 89(2), p268-274.
[https://doi.org/10.1067/mpr.2003.50]

- Blatz, MB, Sadan, A, Arch, GH, Lang, BR, (2003), In vitro evaluation of long-term bonding of Porcera all-ceram alumina restorations with modified resin luting cement, J Prosthet Dent, 89(4), p381-387.
- Blatz, MB, Chiche, G, Holst, S, Sadan, A, (2007), Influence of surface treatment and simulated aging on bond strengths of luting agents to zirconia, Quintessence Int, 38(9), p745-753.
-
Canay, Ş, Hersek, N, Ertan, A, (2001), Effect of different acid treatments on a porcelain surface 1, J Oral Rehabil, 28(1), p95-101.
[https://doi.org/10.1046/j.1365-2842.2001.00626.x]

- Craig, RG, (1989), Restorative dental materials, Mosby, St. Louis, CV, p65.
-
Denry, I, Kelly, JR, (2008), State of the art of zirconia for dental applications, Dent Mater, 24(3), p29-307.
[https://doi.org/10.1016/j.dental.2007.05.007]

- Drummond, JL, Eliades, G, (2003), Ceramic Behavior Under Different Environmental and Loading Conditions. Dental Materials In Vivo: Aging and Related Phenomena. Chicago, IL, Quintessence Int, p35-45.
-
Fischer, H, Niedhart, C, Kaltenborn, N, Prange, A, Marx, R, Niethard, FU, Telle, R, (2005), Bioactivation of inert alumina ceramics by hydroxylation, Biomaterial J, 26(31), p6151-6157.
[https://doi.org/10.1016/j.biomaterials.2005.04.038]

-
Fischer, J, Stawarczyr, B, Hammerle, (2008), Flexural strength of veneering ceramic for zirconia, J Dentis, 36, p316-321.
[https://doi.org/10.1016/j.jdent.2008.01.017]

- Galoppini, E, (2004), Linkers of anchoring sensitizers to semiconductor nano-particles, Coord Chem Rew, 284, p1283-1297.
- ISO 9693, Metal-ceramic dental restorative system, (2009).
- Jeoung, SH, Bae, JM, Oh, (2012), Effect of chemical treatment on the bond strength between zirconia and veneer ceramics, J Korean Res Soc Dent Mater, 39(4), p269-276.
-
Kokubo, T, Kim, HM, Kawashita, M, (2003), Novel bioactive materials with different mechanical properties, Biomaterial J, 24(13), p2161-2175.
[https://doi.org/10.1016/S0142-9612(03)00044-9]

-
Lawn, BR, Pajares, A, Zhang, Y, Deng, Y, Polack, MA, Lloyd, IK, Rekow, ED, Thompson, VP, (2004), Materials design in the performance of all-ceramic crowns, Biomaterial J, 25(14), p2885-2892.
[https://doi.org/10.1016/j.biomaterials.2003.09.050]

-
Lohbauer, U, Zipperle, M, Rischka, K, Petschelt, A, Muller, FA, (2008), Hydroxylation of dental zirconia surfaces: characterization and bonding potential, J Biomed Mater Res B Appl Biomater, 87(2), p461-467.
[https://doi.org/10.1002/jbm.b.31126]

-
Piascik, JR, Wolter, SD, Stoner, BR, (2011), Development of a novel surface modification for improved bonding to zirconia, Dent Mater, 27(5), p99-105.
[https://doi.org/10.1016/j.dental.2011.01.005]

- Rosenstiel, SF, Land, MF, Fujimoto, J, (2001), Contemporary Fixed Prosthodontics, Mosby, St. Louis, MO, p262-271.
-
Sjogren, G, Sletten, G, Dahl, JE, (2000), Cytotoxicity of dental alloys, metals, and ceramics assesse by millipore filter, agar overlay, and MTT tests, J Prosthet Dent, 84(2), p229-236.
[https://doi.org/10.1067/mpr.2000.107227]

- Strub, JR, Beschnidt, SM, (1998), Fracture strength of 5 different all-ceramic crown systems, Int J Prosthodont, 11(6), p602-609.
-
Swain, MV, (2009), Unstable cracking (chipping) of veneering porcelain on all-ceramic dental crowns and fixed partial dentures, Acta Biomater, 5(5), p1668-1677.
[https://doi.org/10.1016/j.actbio.2008.12.016]

- Touzi, H, Chevalier, Y, Kalfat, R, Quada, HB, Zarrouk, H, Chapel, JP, Jaffrezic Renault, N, (2006), Elaboration and electrical characterization of silicone-based anionexchage materials, Mate Sci Eng C, 48, p1347-1354.
-
Uchida, M, Kim, HM, Kokubo, T, Nawa, M, Asano, T, Tanaka, K, Nakamura, T, (2002), Apatite-forming ability of a zirconia/alumina nano-composite induced by chemical treatment, J Biomed Mater Res, 60(2), p277-282.
[https://doi.org/10.1002/jbm.10071]

- Wedler, G, (2004), Lehrbuch Der Physikalischen Chemie, 5th ed, VCH-wiley, New York.
- Zahran, M, El-Mowafy, O, Tam, L, Watson, Pa, finer, Y, (2008), Fracture strength and fatigue resistanc of allceramic molar crowns manufactured with CAD/CAM technology, Int J Prosthodont, 17(5), p370-377.
- Zarone, F, Russo, S, Sorrentino, R, (2011), From porcelainfused- to-metal to zirconia: clinical an experimenta considerations, Dent Mater, 27(1), p83-96.