Comparison of Setting Time, Compressive Strength, Solubility, and pH of Four Kinds of MTA
 ; Seon-Mi Kim1 ; Nam-ki Choi1 ; Hyun-Joo Moon2 ; Moon-Jin Hwang2 ; Ho-Jun Song2 ; Yeong-Joon Park2
; Seon-Mi Kim1 ; Nam-ki Choi1 ; Hyun-Joo Moon2 ; Moon-Jin Hwang2 ; Ho-Jun Song2 ; Yeong-Joon Park2
초록
ProRoot MTA의 단점을 보완하기 위한 mineral trioxide aggregate (MTA)의 다양한 변형제품이 개발되고 있다. 본 연구는 새로운 MTA 제품들의 경화시간, 압축강도, 용해도 및 pH 특성을 ProRoot MTA의 물성과 비교하고자 하였다. 본 연구에서는 ProRoot MTA (Dentsply, USA)를 포함하여 Ortho MTA (BioMTA, Korea), Retro MTA (BioMTA, Korea), 그리고 Endocem MTA (Maruchi, Korea), 이렇게 총 4종의 상용 MTA제품에 대해 평가하였다. 경화시간과 압축강도는 ISO 9917 방법에 따라, 용해도는 ISO 6876 방법에 따라 평가하였으며, pH는 고체시편 전용전극이 연결된 수소이온측정기를 이용하여 측정하였다. Endocem MTA과 Retro MTA의 경화시간은 다른 두 제품들의 경화시간에 비해 유의하게 짧았다(p<0.05). Retro MTA와 ProRoot MTA의 압축강도는 유의한 차이를 보이지 않았고(p>0.05), 이들은 다른 두 제품들에 비해 유의하게 높은 압축강도를 보였다(p<0.05). Endocem MTA는 모든 측정시간 대에 가장 낮은 값을 보였으며, 7일째에 유의한 강도증가를 보였다(p<0.05). Ortho MTA의 용해도 (2.393±0.685%)는 실험제품 중 가장 높았으나, 실험제품 모두 ISO표준의 용해도 허용기준인 3%보다 낮아 적합하였다. 실험제품 모두 강알칼리성의 pH값(10~13)을 보였으며, 경화시간이 길어짐에 따라 알칼리성은 감소하였다. Endocem MTA는 혼합 후 10분, 3시간, 6시간 측정 값 모두 실험군 중 가장 낮은 pH값을 보였다 (p<0.05). Retro MTA와 Endocem MTA는 경화시간이 짧아 향상된 물성을 보였고, 알칼리성이 높고 용해도가 낮아서 압축강도가 크게 요구되지 않는 임상케이스에서 단일방문 시술에 사용될 수 있을 것으로 사료된다.
Keywords:
Mineral Trioxide Aggregate키워드:
경화시간, 압축강도, 용해도, 수소이온농도Ⅰ. INTRODUCTION
The key to success in endodontic treatment is hermetic sealing of the root canal to provide an apical seal that inhibits the leakage of irritants from the root canal system into the periradicular tissues. Therefore, ideal materials for endodontic sealing should have adequate sealing ability between the root canal system and its surrounding tissues (Hwang et al., 2001; Torabinejad and Parirokh, 2010). It should also be nontoxic and biocompatible with the host tissue, insoluble in tissue fluids, dimensionally stable, and moisture-resistant (Torabinejad et al., 1993). Since Torabinejad introduced mineral aggregate trioxide (MTA) originally for perforation repair and as a root-end filling material in the 1990s, additional applications in endodontics have been proposed including direct pulp capping, apexification, external root resorption repair, obturation of retained primary teeth, and root canal filling because of its superior sealing ability and biocompatibility (Queiroz et al., 2005; Torabinejad et al., 1995) compared to those of other materials such as amalgam, IRM, super-EBA and gutta-percha (Hwang et al., 2001; O’Connor et al., 1995; Maltezos et al., 2006).
Several modifications of MTA have been marketed since excellent performance of MTA in endodontic treatment was proved. ProRoot MTA (Dentsply, USA) was originally developed in 1998 and used worldwide with the composition of 75% Portland cement, 5% dehydrate calcium sulfate and 20% bismuth oxide (Storm et al., 2008; Schembri et al., 2010). Despite its superior physical (O’Connor et al., 1995; Maltezos et al., 2006) and biological properties (Gandolfi et al., 2010; Aeinehchi et al., 2003; Lee, 2006), ProRoot MTA presents some undesirable characteristics such as long setting time, difficult manipulation and insertion, potential of discoloration and high cost (Torabinejad et al., 1993; Ber et al., 2007; AlAnezi et al., 2011; Belobrov and Parashos, 2011).
Recently, 3 types of modifications of MTA-based materials such as Ortho MTA (BioMTA, Korea), Retro MTA (BioMTA, Korea), and Endocem MTA (Maruchi, Korea), with different proportions and/or components to alleviate those undesirable characteristics, have been developed and subsequently marketed in the early 2010s.
Ortho MTA has similar compositions as ProRoot MTA but less heavy metal contents than ProRoot (Chang et al., 2011; Kim et al., 2012; Kang et al., 2011). The manufacturer claims that Ortho MTA is fine bioceramic powder with a granularity of only 2 microns, which has biocompatible and even bioactive effect to enhance its sealing property and unaffected by moisture or blood contamination (BioMTA, 2013). Retro MTA is ZrO2-contaning calcium aluminate cement that uses hydraulic calcium zirconia complex as its contrast media. According to the manufacturer, Retro MTA does not cause discoloration even in instances of blood contamination. Endocem MTA is an MTA-derived pozzolan cement (Choi et al., 2013; Jang, 2013). According to manufacturer, Endocem sets quickly without the addition of a chemical accelerator because it contains small particle pozzolan cement (Maruchi, 2013).
However, adding or removing elements in various components of MTA to alleviate main drawbacks could affect other characteristics for clinical success. Many studies have reported that new formula with hydration accelerators to overcome long setting time, one of the major disadvantages of those materials, resulted in diverse influences regarding other physical properties such as compressive strength, solubility and pH (Kogan et al., 2006; Jeong et al., 2010; Lee et al., 2011).
Introducing new MTA with tailored compositions and/or formulations clearly needs comprehensive investigations to support their suitability for clinical uses in endodontic applications. However, few studies have been investigated on recently marketed MTA compared to originally introduced MTA (ProRoot MTA). The aim of this study was to compare the setting time, compressive strength, solubility and pH of Ortho MTA, Retro MTA and Endocem MTA to those of ProRoot MTA.
Ⅱ. MATERIALS AND METHODS
1. Sample Preparation
Four commercial products (Table 1) were used: ProRoot MTA (Dentsply, USA), Ortho MTA (BioMTA, Korea), Retro MTA (BioMTA, Korea), and Endocem MTA (Maruchi, Korea).
2. Setting Time
The setting times of test materials were determined according to the ISO 9917 method (International Organization for Standardization, 2007) with a Vicat apparatus. The Vicat indenter is 400 ± 5 g in weight with a needle having a flat end of 1.0 ± 0.1 mm in diameter. Each material was mixed and placed in a circular acrylic mold (10 mm of inner diameter and 5 mm of height). The assembly was placed in a cabinet at 37oC and relative humidity of 95%. Ninety seconds after the end of mixing, the indenter needle was carefully lowered vertically on to the surface of the material and allowed to remain there for 5 seconds. To determine the approximate setting time, the indentations were repeated at 30 seconds intervals until the needle fails to make a complete circular indentation in the test material. This process was repeated starting the indentation at 30 seconds before the approximate setting time thus determined, making indentations at 10 seconds intervals. This test was repeated 5 times for each material.
3. Compressive Strength
The compressive strengths of the test materials were determined by the method of the ISO 9917 (International Organization for Standardization, 2007). Each material was mixed and placed in split stainless steel molds (internal dimensions 6.0 ± 0.1 mm high and 4.0 ± 0.1 mm of internal diameter). No later than 120 seconds after the end of mixing, the whole assembly was transferred to the cabinet maintained at 37oC for 6 hours. The specimens were removed from the molds and checked visually for air voids or chipped edges. Any such defective specimens were discarded. The specimens were immersed in distilled water for 24 hours, 3 days, and 7 days and maintained at 37oC. Then their compressive strengths were measured using a universal testing machine (Instron, Model GB/4302, Instron Corp., High Wycombe, UK) at a crosshead speed of 1.0 mm/min. The maximum load required to fracture each specimen was measured and the compressive strength (C) was calculated in megapascals according to the formula.
C = 4P / πD2
Where, P is the maximum load applied in Newton and D is the mean diameter of the specimen in millimeters. This test was repeated 5 times for each material.
4. Solubility
The solubility of the test materials was assessed in accordance with the ISO 6876 standard (International Organization for Standardization, 2001). Each material was mixed and placed in two split-ring molds (internal diameter 20 ± 1 mm, 1.5 ± 0.1 mm high). The filled molds were placed in a cabinet maintained at 37oC and a relative humidity of 95% for a period of time 50% longer than the setting time. The specimens were removed from the molds and the mass of each specimen was determined to the nearest 0.001 g with a precision scale (A200S, Sartorius, Goettingen, Germany; precision = 0.0001 g). Two specimens were placed in the shallow dish and 50 ± 1 mL of distilled water was added. The dish was covered and placed in a cabinet for 24 hours. The specimens were removed and washed with 2-3 mL of fresh water, recovering the washings in a shallow dish. The water was then evaporated from the dish without boiling and dried to constant mass at 110 ± 2oC. After cooled, the dish was weighed. The differences found between this weight and the original dish weight were divided into the initial dry weight of the specimens and multiplied by 100. The result was recorded as solubility. This test was repeated 3 times for each material.
5. pH
The test material was mixed and placed in circular Teflon mold (11 mm of inner diameter, 2 mm of height). The pH was measured with a pH meter (Delta350, Mettler Toledo, Schwerzenbach, Switzerland) using an electrode for solid specimen (InLab Surface, Mettler Toledo, Schwerzenbach, Switzerland) at the end of mixing, after 10 minutes, 3 hours, 6 hours, and 24 hours. The apparatus was previously calibrated with pH 9.21, pH 7.0 and pH 4.01 solutions. Between each measurement the electrode was washed with distilled water and blot dried. This test was repeated 5 times for each material.
6. Statistical Analysis
All data from repeated tests are expressed as the mean ± standard deviation. One way analysis of variance followed by Tukey's Post Hoc test was used to determine any statistical differences in setting time, compressive strength, solubility, and pH between the various mixtures. A p-value of less than 0.05 was considered statistically significant.
Ⅲ. RESULTS
1. Setting Time
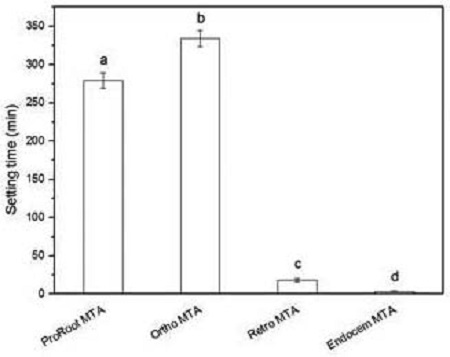
The setting times of test materials are summarized in Table 2 and Figure 1. The setting times for Ortho MTA, ProRoot MTA, Retro MTA, and ENDOCEM MTA were 334.4 min, 279.0 min, 18.1 min, and 3.6 min, respectively (p<0.05). Especially the setting time of Endocem MTA and Retro MTA were shorter than the others.
2. Compressive Strength
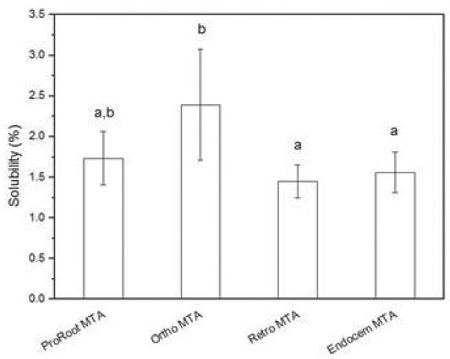
The compressive strengths (MPa) of the test materials at different times are summarized in Table 3 and Figure 2. Compressive strengths of Retro MTA and ProRoot MTA were significantly higher than the other two at all measuring time points (p<0.05). Endocem MTA showed significantly lower compressive strength (Endocem MTA: 1 day; 8.90±1.15, 3 days; 10.66±0.97, 7 days; 16.25±2.96 MPa) than those of other materials (p<0.05).
Compressive strength (MPa) of the tested materials (n = 5).*Between tested materials at same time point, mean values with the same superscript alphabet are not significantly different (p>0.05).**Within same material, mean values with the same superscript number are not significantly different (p>0.05).
3. Solubility
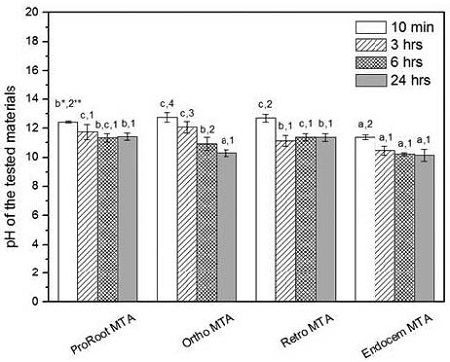
The solubility in water of the test materials are summarized in Table 4 and Figure 3. Solubility of Ortho MTA (2.393±0.685%) was the highest one (p<0.05), and the other materials showed as ProRoot MTA (1.735± 0.328%), Endocem MTA (1.561±0.253%), and Retro MTA (1.447± 0.201%) (p>0.05).
4. pH
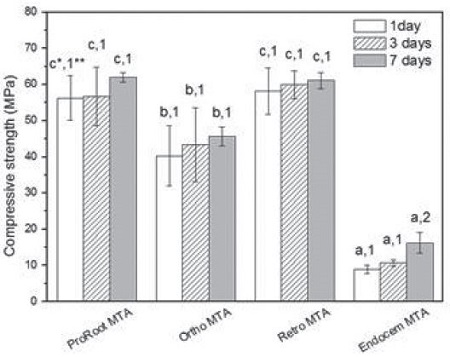
The pH of the test materials at different time points are summarized in Table 5 and Figure 4. The pH of all the tested materials showed similar values of pH 10~13, and decreased as the specimens age from 10 min to 3 hr (p<0.05). After 3 hours, all the materials, except Retro MTA, showed insignificant decrease of pH (p>0.05). The Retro MTA, ProRoot MTA, and Ortho MTA, which showed longer setting time, had significantly higher pH values compared to Endocem MTA, which showed shortest setting time, at all the test time points (except for Ortho MTA vs. Endocem MTA at 24 hours: p>0.05).
Ⅳ. DISCUSSION
1. Setting Time
All the materials evaluated in this study are MTA-based materials supplied as a very fine inorganic hydrophilic powder, which are mixed with water, and set primarily by hydration reaction. Hydration of MTA powder results in a colloidal gel that solidifies into a hard structure. Overall setting behaviors of MTA have been demonstrated in previous studies. The setting of MTA occurs in three stages. In the first 24 hours, the tricalcium aluminate hydrates to form hydrated colloidal gel of tricalcium aluminate. The second phase occurs between the 1st and 7th days. The tricalcium silicates and tricalcium aluminate react with water to form calcium hydroxide, aluminum hydroxide, and amorphous calcium silicate. The third phase of cement setting is a slow reaction and occurs between the 7th and 28th days. During that period the calcium silicates progressively hydrate to form hydrated silicate gel, and calcium hydroxide becomes studded in this gel, imparting strength to the set cement.
When MTA is mixed with water in this study, the cement undergoes a continuous transformation from fluid to a solid state. In this study, the solidification state was measured using a penetration test, such as the Vicat apparatus. The setting time of ProRoot MTA and Ortho MTA were 279.0 min and 334.4 min, respectively (Table 2, Figure 1). There is a discrepancy in setting time for ProRoot MTA and Ortho MTA between our results and other recent investigations that demonstrated to be 175-202 min (Ber et al., 2007; AlAnezi et al., 2011; Chng et al., 2005) and 307 min (Kang et al., 2011), respectively. To determine the approximate setting time, the indentations were repeatedly penetrated at 30 seconds intervals until the needle fails to make a complete circular indentation in the test material. The difference in the weight of the indentation used in these tests and the sensitivity of the different testing apparatus may contribute to these discrepancies.
In this study, the setting time of Endocem MTA and Retro MTA were 3.6 min and 18.1 min, respectively, which were significantly shorter than that of ProRoot MTA and Ortho MTA (p<0.05). The results of these two materials supported the manufacturers’ claims as a fast setting product. The long setting time of MTA is one of the reasons that MTA could not be applied in single-visit. when a slow setting MTA is placed against tissue, it might be washed out by body flow (Ko, 2010; Lee et al., 2010). Based on our results, Retro MTA and Endocem MTA could be recommended for single-visit procedures where other properties are not a major concern.
The development of fast-setting MTA has been attempted by many researchers (Kogan et al., 2006; Jeong et al., 2010; Lee et al., 2011). However, most of these approaches were based on the addition of chemical setting accelerators, some of which showed adverse physical and biological effects. Recently, Endocem MTA, a fast-setting MTA-derived cement, was developed by using small particles of pozzolan cement without any chemical accelerators (Jang, 2013). A pozzolan is a siliceous or siliceous and aluminous material that possesses little or no cementitious value in itself, but it will react chemically with calcium hydroxide in finely divided form and in the presence of water at ordinary temperature to form compounds possessing cementitious properties (Jang, 2013).
2. Compressive Strength
Compressive strengths of Retro MTA and ProRoot MTA were higher than those of the other two materials at all measuring time points (p<0.05). Endocem MTA showed significantly lower compressive strength than those of other materials (p<0.05)(Table 3, Figure 2). The compressive strength is another important property that needs to be considered in addition to setting time. Retro MTA and Endocem MTA, which are fast setting, showed distinct results in compressive strength. While Retro MTA showed the highest values similar to ProRoot MTA, Endocem MTA showed the lowest values at all the test periods (p>0.05). On the basis of manufacturer data sheet, Ortho MTA and Retro MTA have finer particles in comparison to ProRoot MTA. Small particle sizes might increase surface contact with mixing liquid and lead to greater early strength as well as ease of handling characteristics. However, many studies have reported that new formula to overcome long setting time resulted in diverse results in compressive strength. Kogan (Kogan et al., 2006) reported that addition of NaOCl gel, K-Y Jelly, and 5% CaCl2 to MTA as hydration accelerators improved setting time. However, they also reduced the compressive strengths.
Considering the clinical applications, the difference in compressive strength of the MTA may favor its different usefulness. When MTA is used for perforation repairs and where additional forces will be applied to the set material, as with amalgam core build-ups, high compressive strength of the MTA is desired. The clinician would either use a mixture with a higher compressive strength or protect the MTA with a barrier that possesses higher compressive strength. On the other hand, when the MTA is used as a root-end filling material, the clinician may favor a material that has a rapid setting time to decrease the possible washout. Reduced compressive strength will not be a major drawback since minimal forces are applied to the retro-filling materials.
3. Solubility
Ortho MTA showed the highest solubility value of 2.393±0.685%, and the other three materials showed similar values as ProRoot MTA (1.735± 0.328%), Endocem MTA (1.561±0.253%), and Retro MTA (1.447± 0.201%) (p>0.05)(Table 4, Figure 3).
After endodontic surgery, the retrograde-filled MTA that is not set may encounter blood or tissue fluid. Kim et al (Kim et al., 2012) reported that washout of MTA could be mediated by continuous flow of exudates or tissue fluid. Although MTA has excellent sealing ability, its washout can prevent the complete sealing of the retrograde preparation site and thus eventually cause failure (Kim et al., 2012; Choi et al., 2013).
The powder-to-water ratio might influence the amount of solubility. In fact, higher water-to-powder ratios increased MTA porosity and solubility. The addition of bismuth oxide to MTA, which is insoluble in water, is another cause for MTA insolubility. These findings are in contrast with another study that shows Retro MTA is less soluble than the other types of MTA.
In an investigation on the solubility of MTA in comparison to polycarboxylate cements, all the tested materials showed less than 3% weight loss during 24hours after mixing, which is lesser that acceptable weight loss specified by the ISO (International Organization for Standardization, 2001) and American Dental Association. Slow setting time may be one of the reasons for the greater solubility of Ortho MTA, and it is likely that the rapid setting of Retro MTA and Endocem MTA might enhance their washout resistance.
4. pH
The pH changes were measured at 10 min, 3 h, 6 h and 24 h after end of mixing. The results showed a strong alkaline pH of 11-13 at 10 min, with a tendency of reduction in alkalinity after longer periods, and finally reached to 10-12 at 24 h, where Endocem MTA showed the lowest pH value among the tested materials at all measuring time points (Table 5, Figure 4).
When comparing pH values at different periods of time, statistical differences between 10 min and 3 hours were noted for all materials. After 3 hours, however, except Ortho MTA, there was no significant decrease of pH (p>0.05).
With regard to the pH values, a maximum value of 12.43 for ProRoot MTA at the initial setting periods was observed, similar to the previous studies of Torabinejard et al. (Torabinejad and Parirokh, 2010) and Lee et al. (Lee et al., 2011) which showed values higher than 12.0. These results show that mixing MTA with water results in the formation of calcium hydroxide and a high pH environment.
It is known that calcium oxide in the material composition would probably react with the tissue fluids and produce calcium hydroxide, which in turn would dissociate into hydroxide and calcium ions. The hydroxide ions would be responsible for the high pH environment, and consequently for the activation of alkaline phosphatase (de Vasconcelos et al., 2009). With strong alkalinity of these materials, clinically applied MTA would probably alleviate necrosis of resorptive cells on the root surface and may also be bactericidal.
The Retro MTA, ProRoot MTA, and Ortho MTA which showed longer setting time had significantly higher pH values compared to Endocem MTA which showed shortest setting time, at all the test time points (except for Ortho MTA vs. Endocem MTA at 24 hours: p>0.05). All the tested cements showed alkaline pH with a tendency of reduction in alkalinity at longer periods.
Ⅴ. CONCLUSION
Retro MTA has similar properties in compressive strength and solubility compared to ProRoot MTA. The setting time of Retro MTA and Endocem MTA was shorter than ProRoot MTA. Because Retro MTA and Endocem MTA presented improved setting time and low solubility, this combination may be an alternative choice in single visit procedures where compressive strength of the material is not a critical issue. Further chemical properties and biocompatibility in vitro and in vivo should be evaluated to determine the suitability of modified MTA products for clinical use. Methods to improve the setting property and compressive strength are also required to be explored for the expanded clinical application of MTA products.
Conflict of interest
The authors deny any conflicts of interest related to this study.
Acknowledgments
This study was financially supported by the National Research Foundation of Korea (NRF) grant funded by the Korea Government (MSIP) (No. 2011-0030121).
References
-
Aeinehchi, M., Eslami, B., Ghanbariha, M., Saffar, AS., (2003), Mineral trioxide aggregate (MTA) and calcium hydroxide as pulp-capping agents in human teeth: a preliminary report, Int Endod J, 36, p225-231.
[https://doi.org/10.1046/j.1365-2591.2003.00652.x]

-
AlAnezi, AZ., Zhu, Q., Wang, YH., Safavi, KE., Jiang, J., (2011), Effect of selected accelerants on setting time and biocompatibility of mineral trioxide aggregate (MTA), Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 111, p122-127.
[https://doi.org/10.1016/j.tripleo.2010.07.013]

-
Belobrov, I., Parashos, P., (2011), Treatment of tooth discoloration after the use of white mineral trioxide aggregate, J Endod, 37, p1017-1020.
[https://doi.org/10.1016/j.joen.2011.04.003]

-
Ber, BS., Hatton, JF., Stewart, GP., (2007), Chemical modification of ProRoot MTA to improve handling characteristics and decrease setting time, J Endod, 33, p1231-1234.
[https://doi.org/10.1016/j.joen.2007.06.012]

- BioMTA, Available from URL: http://www.biomta.com/shop/eng/product (Accessed on December 12, 2013).
-
Chang, SW., Baek, SH., Yang, HC., Seo, DG., Hong, ST., Han, SH., Lee, Y., Gu, Y., Kwon, HB., Lee, W., Bae, KS., Kum, KY., (2011), Heavy metal analysis of Ortho MTA and ProRoot MTA, J Endod, 37, p1673-1676.
[https://doi.org/10.1016/j.joen.2011.08.020]

-
Chng, HK., Islam, I., Yap, AU., Tong, YW., Koh, ET., (2005), Properties of a new root-end filling material, J Endod, 31, p665-668.
[https://doi.org/10.1097/01.don.0000157993.89164.be]

-
Choi, YRN., Park, SJ., Lee, SH., Hwang, YC., Yu, MK., Min, KS., (2013), Biological effects and wash-out resistance of a newly developed fast-setting mineral trioxide aggregate, J Endod, 39, p467-472.
[https://doi.org/10.1016/j.joen.2012.11.023]

-
Gandolfi, MG., Taddei, P., Tinti, A., Prati, C., (2010), Apatite-forming ability (bioactivity) of ProRoot MTA, Int Endod J, 43, p917-929.
[https://doi.org/10.1111/j.1365-2591.2010.01768.x]

- Hwang, YC., Kang, IC., Hwang, IN., Oh, WM., (2001), Comparison of the sealing ability of various retrograde filling materials, J Korean Acad Pediatr Dent, 26, p379-386.
- International Organization for Standardization, (2001), ISO 6876: dentistry - dental root canal sealing materials, Geneva, Switzerland, ISO.
- International Organization for Standardization, (2007), ISO 9917-1: dentistry - water-based cements - part 1: powder/liquid acid-base cements, Geneva, Switzerland, ISO.
- Jang, KY., (2013), Effects of various root canal irrigants on washout resistance of fast-setting pozzolan cement, (Master’s thesis), Wonkwang University, Iksan, Korea.
-
Jeong, YN., Yang, SY., Park, BJ., Park, YJ., Hwang, YC., Hwang, IN., Oh, WM., (2010), Physical and chemical properties of experimental mixture of mineral trioxide aggregate and glass ionomer cement, J Korean Acad Cons Dent, 35, p344-351.
[https://doi.org/10.5395/JKACD.2010.35.5.344]

-
Kang, JY., Kim, JS., Yoo, SH., (2011), Comparison of setting expansion and time of Ortho MTA, ProRoot MTA and Portland cement, J Korean Acad Pediatr Dent, 38, p229-236.
[https://doi.org/10.5933/JKAPD.2011.38.3.229]

-
Kim, SY., Choi, NK., Park, JI., Kim, SM., (2012), Comparison of antimicrobial effects of Ortho MTA and ProRoot MTA, J Korean Acad Pediatr Dent, 39, p366-372.
[https://doi.org/10.5933/JKAPD.2012.39.4.366]

- Ko, HJ., (2010), The myths and facts of MTA, J Korean Dent Assoc, 48, p813-818.
-
Kogan, P., He, J., Glickman, GN., Watanabe, I., (2006), The effects of various additives on setting properties of MTA, J Endod, 32, p569-572.
[https://doi.org/10.1016/j.joen.2005.08.006]

-
Lee, BN., Hwang, YC., Jang, JH., Chang, HS., Hwang, IN., Yang, SY., Park, YJ., Son, HH., Oh, WM., (2011), Improvement of the properties of mineral trioxide aggregate by mixing with hydration accelerators, J Endod, 37, p1433-1436.
[https://doi.org/10.1016/j.joen.2011.06.013]

-
Lee, SJ., Cho, OI., Yum, JW., Park, JK., Hur, B., Kim, HC., (2010), Physical properties of novel composite using Portland cement for retro-filling material, J Korean Acad Cons Dent, 35, p445-452.
[https://doi.org/10.5395/JKACD.2010.35.6.445]

- Lee, SM., (2006), Histologic evaluation of MTA as pulpotomy and pulp capping agent, (Masters dissertation), Chosun University, Gwangju, Korea.
-
Maltezos, C., Glickman, GN., Ezzo, P., He, J., (2006), Comparison of the sealing of Resilon, ProRoot MTA, and Super-EBA as root-end filling materials: a bacterial leakage study, J Endod, 32, p324-327.
[https://doi.org/10.1016/j.joen.2005.08.015]

- Maruchi, Available from URL: http://www.endocem.com/maruchi/shop/item (Accessed on December 12, 2015).
-
O'Connor, RP., Hutter, JW., Roahen, JO., (1995), Leakage of amalgam and Super-EBA root-end fillings using two preparation techniques and surgical microscopy, J Endod, 21, p74-78.
[https://doi.org/10.1016/S0099-2399(06)81099-X]

-
Queiroz, AM., Assed, S., Leonardo, MR., Nelson-Filho, P., Silva, LA., (2005), MTA and calcium hydroxide for pulp capping, J Appl Oral Sci, 13, p126-130.
[https://doi.org/10.1590/S1678-77572005000200006]

-
Schembri, M., Peplow, G., Camilleri, J., (2010), Analyses of heavy metals in mineral trioxide aggregate and Portland cement, J Endod, 36, p1210-1215.
[https://doi.org/10.1016/j.joen.2010.02.011]

-
Storm, B., Eichmiller, FC., Tordik, PA., Goodell, GG., (2008), Setting expansion of gray and white mineral trioxide aggregate and Portland cement, J Endod, 34, p80-82.
[https://doi.org/10.1016/j.joen.2007.10.006]

-
Torabinejad, M., Hong, CU., McDonald, F., Pitt Ford, TR., (1995), Physical and chemical properties of a new root-end filling material, J Endod, 21, p349-353.
[https://doi.org/10.1016/S0099-2399(06)80967-2]

-
Torabinejad, M., Parirokh, M., (2010), Mineral trioxide aggregate; a comprehensive literature review –part 2: leakage and biocompatibility investigations, J Endod, 36, p190-202.
[https://doi.org/10.1016/j.joen.2009.09.010]

-
Torabinejad, M., Watson, TF., Pitt Ford, TR., (1993), Sealing ability of a mineral trioxide aggregate when used as a root end filling material, J Endod, 19, p591-595.
[https://doi.org/10.1016/S0099-2399(06)80271-2]

-
Torabinejad, M., Parirokh, M., (2010), Mineral trioxide aggregate; a comprehensive literature review –part 2: leakage and biocompatibility investigations, J Endod, 36, p190-202.
[https://doi.org/10.1016/j.joen.2009.09.010]

-
de Vasconcelos, BC., Bernardes, RA., Cruz, SML., Duarte, MA., Padilha, PM., Bernardineli, N., Garcia, RB., Bramante, CM., de Moraes, IG., (2009), Evaluation of pH and calcium ion release of new root-end filling materials, Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 108, p135-139.
[https://doi.org/10.1016/j.tripleo.2009.02.026]