Effect of the 457 nm Laser on the Bond Strength of Orthodontic Brackets
초록
본 연구는 457 nm 레이저가 교정용 브라켓의 전단결합강도에 미치는 영향을 평가하였다. 본 연구에서는 3종의 수복용 복합레진 (Filtek Z350, Filtek Z250 및 Filtek Z350 flow)과 Transbond XT를 접착제로 사용하였고, 457 nm 레이저 (LVI-VA457-100)와 2종의 광조사기 (Optilux 501, L.E.Demetron)를 사용하였다. 교정용 브라켓을 발거된 상악소구치에 부착하고 광조사한 후, 광중합이 완료된 시료의 결합강도를 측정하고 파절면을 관찰하였다. 그 결과 광조사기군에서는 통계적으로 유의한 차이는 나타나지 않았다. 반면, 접착제군에서는 통계적으로 유의한 차이가 나타났으며, Transbond XT군이 (14.17 ± 2.53-16.56 ± 2.89 MPa) 다른 복합레진군보다 (13.04 ± 1.68-14.59 ± 2.89 MPa) 높은 결합강도를 보였다. 시편의 반 정도는 (42%-LED, 42%-QTH, 및 52%-457 nm laser) 치아-접착제 계면 파절을 보였으며, 나머지 반을 접착제 내에서 파절이 발생하였다. 결론적으로 457 nm 레이저는 QTH (Optilux 501)나 LED (L.E.Demetron) 광조사기와 마찬가지로 교정용 브라켓을 부착 시 광조사기로 사용될 수 있다는 것을 확인하였다.
Keywords:
457 nm laser, Shear bond strength, Light-curing units, AdhesivesⅠ. INTRODUCTION
Demand for esthetics has resulted in increased interest of orthodontics. In particular, acid etching of tooth surfaces and direct bonding techniques is now widely used in contemporary orthodontic practice (Tabrizi et al., 2010). Chemical- and light-curing adhesive systems are largely chosen according to the best handling characteristics, and light-curing orthodontic adhesives are becoming more popular because of the advantage of high early bond strength and sufficient working time to enable practitioners to position brackets accurately (Trimpeneers et al., 1996)
As a light source for curing of resin adhesive, several light-curing units (LCUs) have been introduced to the market. Quartz-tungsten-halogen (QTH) units have been used as the standard despite their disadvantages such as high levels of heat generation and limited lifespans (Strydom, 2005). On the other hand, light-emitting diodes (LEDs) generate less heat than conventional QTH units (Mills et al., 2002; Bala et al., 2005), have long lifespans, and emit light at high intensities. Plasma arc units were claimed to allow complete curing in 3 seconds due their high intensities (Katahira et al., 2004), but were found to achieve incomplete polymerization due to the insufficient curing time (Price et al., 2005).
Lasers are highly attractive and valuable light source due to their exceptional characteristics, such as monochromaticity and coherence, compared with other light sources. Due to these favorable features, many lasers have been challenged on the application in dentistry after the initial development of the laser in 1960s. Among them, the argon laser was widely tested for curing photoinitiator- containing composite resins and bonding adhesive (Elvebak et al., 2006; Ramos Lloret et al., 2008; Turbino et al., 2011; Mirsasaani et al., 2013). One major emission peak (488 nm) of the argon laser matches with the absorption band (approximately 463 nm) of principal photoinitiator (camphorquinone, CQ). However, high price and bulky size limited the argon laser to be widely adopted in local clinics. Among the recently developed lasers, a laser of 457 nm can be useful because it closely matches with the absorption peak of CQ and is of handy size and economic price, it needs to be challenged.
When an orthodontic bracket is bonded, the bond strength should be high enough to withstand masticatory and archwire stresses. The bond strength of bracket is mainly influenced by the adhesive used, but LCUs can also affect bond strengths. Several studies have been conducted on shear bond strengths (SBS) obtained using different LCUs (Lalani et al., 2000; Klocke et al., 2003; Di Nicoló et al., 2010; Cerekja and Cakirer, 2011), but no study has yet addressed the possibility of using the 457 nm laser as a light source for bracket bonding. Accordingly, the purpose of this study was to investigate the effectiveness of the 457 nm laser for the bonding of orthodontic brackets.
Ⅱ. MATERIALS AND METHODS
1. Adhesives and LCUs
A total of 180 caries-free human maxillary premolars were collected and stored in 0.2 per cent thymol solution. After eliminating all soft tissues and extraneous material, teeth were pumiced with a polishing paste for 10 seconds and rinsed in tap water for 20 seconds.
Three different restorative composite resins were tested during the SBS evaluation: Filtek Z350 (nanocomposite resin), Filtek Z250 (microhybrid resin), and Filtek Z350 flow (flowable resin). An orthodontic adhesive (Transbond XT) served as a control. Compositional details are shown in Table 1. For light curing, three different LCUs were used: a QTH unit (Optilux 501; Kerr, Danbury, CT, USA), a LED unit (L.E.Demetron; Kerr, Danbury, CT, USA), and a 457 nm laser (LVI-VA457-100; LVI Tech., Seoul, Korea). The output intensities of the QTH and LED units were approximately 900 mW/cm2(measured using a built-in radiometer). The output power (measured using a power meter; PM3/FIELDMAX, Coherent, Portland, OR, USA), spot size, and light intensity of the laser were 150 mW, 5 mm, and approximately 764 mW/cm2, respectively.
2. Bracket bonding conditions
For a bracket bonding test, premolars were randomly divided into twelve groups (four adhesives×three LCUs) containing 15 teeth per group. A metal bracket (Tomy, Tokyo, Japan) was chosen for this study. The metal bracket was for premolars and had 0.018-in slot. The average surface area of bracket base was 12.89 mm2 (the average of five brackets). The metal bracket was bonded to the tooth surface according to manufacturer’s instructions. The tooth were etched with 37 per cent phosphoric acid gel (SCOTCHBOND ETCHANT, 3M Espe, US) for 20 seconds, rinsed, and dried for 15 seconds, and a primer (Transbond XT, 3M Unitek, Monrovia, CA, USA) was uniformly applied to the tooth surface. One resin cement and three composite resins were applied to the bracket base. The bracket was positioned on the tooth surface and 200 g of pressure was applied to the brackets. Excess adhesive was then carefully removed, and light curing was carried out for 40 seconds (distal 20 seconds/mesial 20 seconds). While bonding the brackets to the teeth, the light guide or laser beam was made to face the bracket at an angle of 90°. In order to minimize light loss by beam divergence (in the case of QTH and LED LCUs), the light guide (diameter: 7 mm) was positioned stationary as close as possible to the bracket.
3. Bracket debonding and adhesive remnant index (ARI)
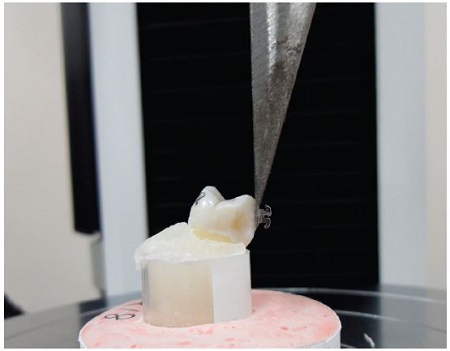
Bracket-bonded specimens were mounted in acrylic resin (orthodontic resin, Dentsply Caulk, US) and stored in distilled water for 24 hours at 37℃ in a dark chamber. SBS was then measured using a universal testing machine (Instron 3345, Instron Corporation, Canton, MA, USA) by applying a shear force along the occlusogingival direction at a crosshead speed of 1 mm/minute (Figure 1). Maximum debonding load was recorded in Newtons (N) and converted to megapascals (MPa) by dividing the maximum load by the surface area of bracket base. After debonding, adhesive remnant index (ARI) was determined using a stereoscopic microscope at a magnification of 10× using the following scoring system: 1 = all adhesive remained on the tested tooth; 2 = > 90 per cent of adhesive remaining; 3 = between 10-90 per cent of adhesive remaining; 4 = <10 per cent of adhesive remaining; and 5 = no adhesive remaining (Bishara at al., 2006).
4. Statistical Analysis
Two-way ANOVA and one-way ANOVA were used to determine the significance of differences between group SBS values (of adhesives and LCUs). The post hoc Tukey test was used for multiple comparisons, and the Kruskal-Wallis test was used to determine the significances of intergroup ARI score differences. Statistical significance was accepted for P values of < 0.05.
Ⅲ. RESULTS
Table 2 shows results of the two-way ANOVA for the different LCU/adhesive combinations. The mean and SD of the SBS values of the different LCU/adhesive groups are shown in Table 3. The two-way ANOVA showed that there were no statistically significant differences in SBS values among the LCU groups (P > 0.05). Analysis of the effect of varying LCU to the adhesive using one-way ANOVA showed that LCU was no significant variable (P > 0.05). However, there were statistically significant differences in SBS values among the composite resins or between Transbond XT and the composite resins (P < 0.001).
The ARI scores for the different LCU/adhesive combinations are detailed in Table 4. Statistical analysis (Kruskal-Wallis test) showed that all test groups exhibited no statistically significant difference in bracket failure modes for adhesive and LCU conditions (P > 0.05). Generally, half of the specimens showed a failure at the tooth-adhesive interface (42 per cent of LED, 42 per cent of QTH, and 52 per cent of 457 nm laser) and the remainder showed cohesive failure (debonding within the adhesive).
Ⅳ. DISCUSSION
Attaching a bracket on a tooth surface for orthodontic purpose involves the polymerization of base adhesive by an external light, the resultant bond strength can vary on the selection of adhesive and LCU. Despite the blue light from each LCU for the maximal absorption by CQ, the tested LCUs have an apparent difference between them: width of emission band. Transbond XT is a conventional adhesive that is optimized for bracket bonding. On the other hand, the composite resins tested in the present study are used for restoration purpose. Despite the difference of usage, all these resins contain CQ as a photoinitiator. Bonding brackets with different light source and adhesive may yield different bond strength.
According to the results, there was no significant differences in their SBS values between the 457 nm laser and the other LCUs. Clinically acceptable minimum bracket bond strength ranges between 6 and 8 MPa (Reynolds, 1975), and in the present study, the SBS values of the three tested composite resins were slightly lower than that of Transbond XT (13.04-14.59 MPa vs 14.17-16.56 MPa) depending on LCU, but much higher than the clinically acceptable minimum bond strength. Since Transbond XT is basically produced for bracket bonding, it has been optimized for bonding bracket bases, and thus, has better workability and softness than the three composite resins tested those were produced for restoration purposes.
On the other hand, the flow of a material is very important factor in applying resin cement on the bracket base. However, the SBS values of Filtek Z350 flow, flowable resin, were significantly lower than the other adhesive. It could be due to the lower filler content of Filtek Z350 flow (Uysal et al., 2004; Ryou et al., 2008; Gama et al., 2013). According to previous studies, filler concentration was positively related to SBS (Ostertag et al., 1991; Sunilkumar et al., 2013). However, in the present study, no specific correlation was found between filler content and SBS values.
ARI scores provide a means of assessing debonding modes at bracket-adhesive-tooth interfaces, but no significant differences were found between groups tested. However, despite the lack of significant differences between ARI scores, a consistent trend, such as more residual adhesive on bracket bases (ARI 4 and 5), was observed. According to the studies about debonding, some reports have concluded that cohesive debonding is the primary mode of failure, and others have concluded adhesive debonding (Bishara et al., 1999; Bishara et al., 2001; Velo and Carano, 2002; Trites et al., 2004; Reis et al., 2007; İşman et al., 2012). Depending on the primary failure mode, the resultant outcome can be different. Debonding at the bracket-adhesive interface avoids the risk of enamel damage due to a high SBS, but requires the removal of residues from tooth surfaces with a suitable rotary instrument, which increases the risk of enamel surface damage. On the other hand, when a bracket debonds at the tooth-adhesive interface, less residue remains on the tooth surface, but resultant SBS values are may probably lower. However, in the present study, no significant correlation was found between debonding mode and SBS value.
Thus, the 457 nm laser has a potential as a light source for the curing of dental adhesives including light-curing composite resins.
Ⅴ. CONCLUSION
This study evaluated the possibility of 457 nm laser as a light source on bracket bonding. Within the limitations of this study, the following conclusions were made:
- 1. The 457 nm laser achieved slightly higher SBS values for orthodontic brackets than the QTH and LED units despite its much lower light intensity.
- 2. There was no statistically significant difference in SBS values between the orthodontic adhesive (Transbond XT) and three composite resins.
- 3. The 457 nm laser was found to satisfy the clinically acceptable minimum bracket bond strength.
Acknowledgments
이 논문은 2014년도 부산가톨릭대학교 교내연구비에 의하여 연구되었음.
References
-
Bala, O., Olmez, A., Kalayci, S., (2005), Effect of LED and halogen light curing on polymerization of resin-based composites, J Oral Rehabil, 32, p134-140.
[https://doi.org/10.1111/j.1365-2842.2004.01399.x]

-
Bishara, SE., Gordan, VV., VonWald, L., Jakobsen, JR., (1999), Shear bond strength of composite, glass ionomer, and acidic primer adhesive systems, Am J Orthod Dentofacial Orthop, 115, p24-28.
[https://doi.org/10.1016/S0889-5406(99)70312-4]

- Bishara, SE., Ostby, AW., Ajlouni, R., Laffoon, JF., Warren, JJ., (2006), Early shear bond strength of a one-step self-adhesive on orthodontic brackets, Angle Orthod, 76, p689-693.
- Bishara, SE., VonWald, L., Laffoon, JF., Warren, JJ., (2001), Effect of using a new cyanoacrylate adhesive on the shear bond strength of orthodontic brackets, Angle Orthod, 71, p466-469.
-
Cerekja, E., Cakirer, B., (2011), Effect of short curing times with a high-intensity light-emitting diode or high-power halogen on shear bond strength of metal brackets before and after thermocycling, Angle Orthod, 81, p510-516.
[https://doi.org/10.2319/071810-412.1]

-
Di Nicoló, R., Araujo, MA., Alves, LA., Assunção, e., Souza, RO., Rocha, DM., (2010), Shear bond strength of orthodontic brackets bonded using halogen light and light-emitting diode at different debond times, Braz Oral Res, 24, p64-69.
[https://doi.org/10.1590/S1806-83242010000100011]

- Elvebak, BS., Rossouw, PE., Miller, BH., Buschang, P., Ceen, R., (2006), Orthodontic bonding with varying curing time and light power using an argon laser, Angle Orthod, 76, p837-844.
-
Gama, AC., Moraes, AG., Yamasaki, LC., Loguercio, AD., Carvalho, CN., Bauer, J., (2013), Properties of composite materials used for bracket bonding, Braz Dent J, 24, p279-283.
[https://doi.org/10.1590/0103-6440201302184]

-
İşman, E., Karaarslan, ES., Okşayan, R., Tunçdemır, AR., Üşümez, S., Adanir, N., Cebe, MA., (2012), Inadequate shear bond strengths of self-etch, self-adhesive systems for secure orthodontic bonding, Dent Mater J, 31, p947-953.
[https://doi.org/10.4012/dmj.2012-103]

- Katahira, N., Foxton, RM., Inai, N., Otsuki, M., Tagami, J., (2004), Comparison of PAC and QTH light sources on polymerization of resin composites, Am J Dent, 17, p113-117.
-
Klocke, A., Korbmacher, HM., Huck, LG., Ghosh, J., Kahl-Nieke, B., (2003), Plasma arc curing of ceramic brackets: an evaluation of shear bond strength and debonding characteristics, Am J Orthod Dentofacial Orthop, 124, p309-315.
[https://doi.org/10.1016/S0889-5406(03)00310-X]

- Lalani, N., Foley, TF., Voth, R., Banting, D., Mamandras, A., (2000), Polymerization with the argon laser: curing time and shear bond strength, Angle Orthod, 70, p28-33.
-
Mills, RW., Uhl, A., Jandt, KD., (2002), Optical power outputs, spectra and dental composite depths of cure, obtained with blue light emitting diode (LED) and halogen light curing units (LCUs), Br Dent J, 193, p459-463.
[https://doi.org/10.1038/sj.bdj.4801597]

-
Mirsasaani, SS., Ghomi, F., Hemati, M., Tavasoli, T., (2013), Measurement of solubility and water sorption of dental nanocomposites light cured by argon laser, IEEE Trans Nanobioscience, 12, p41-46.
[https://doi.org/10.1109/TNB.2012.2229468]

-
Ostertag, AJ., Dhuru, VB., Ferguson, DJ., Meyer, RA. Jr, (1991), Shear, torsional, and tensile bond strengths of ceramic brackets using three adhesive filler concentrations, Am J Orthod Dentofacial Orthop, 100, p251-258.
[https://doi.org/10.1016/0889-5406(91)70062-2]

- Price, RB., Ehrnford, L., Andreou, P., Felix, CA., (2003), Comparison of quartz-tungsten halogen light-emitting diode, and plasma arc curing lights, J Adhes Dent, 5, p193-207.
- Ramos Lloret, P., Lacalle Turbino, M., Kawano, Y., Sanchez Aguilera, F., Osorio, R., Toledano, M., (2008), Flexural properties, microleakage, and degree of conversion of a resin polymerized with conventional light and argon laser, Quintessence Int, 39, p581-586.
-
Reis, A., dos Santos, JE., Loguercio, AD., de Oliveira Bauer, JR., (2007), Eighteen-month bracket survival rate: conventional versus self-etch adhesive, Eur J Orthod, 30, p94-99.
[https://doi.org/10.1093/ejo/cjm089]

-
Reynolds, IR., (1975), A review of direct orthodontic bonding, Br J Orthod, 2, p1-8.
[https://doi.org/10.1080/0301228X.1975.11743666]

-
Ryou, DB., Park, HS., Kim, KH., Kwon, TY., (2008), Use of flowable composites for orthodontic bracket bonding, Angle Orthod, 78, p1105-1109.
[https://doi.org/10.2319/013008-51.1]

- Strydom, C., (2005), Prerequisites for proper curing, SADJ, 60, p254-255.
- Sunilkumar, P., Patil, C., H, B., Putturaj, K., Sangolgi, VC., Jayasudha, KJ., (2013), A Comparative Study of the Shear and Tensile Bond Strength using three types of Direct Bonding Adhesives on Stainless Steel Brackets - An In Vitro Study, J Int Oral Health, 5, p26-29.
-
Tabrizi, S., Salemis, E., Usumez, S., (2010), Flowable composites for bondingorthodontic retainers, Angle Orthod, 80, p195-200.
[https://doi.org/10.2319/033007-155.1]

-
Trimpeneers, LM., Verbeeck, RMH., Dermaut, LR., Moors, MG., (1996), Comparative shear bond strength of some orthodontic bonding resins to enamel, Eur J Orthod, 18, p89-95.
[https://doi.org/10.1093/ejo/18.1.89]

-
Trites, B., Foley, TF., Banting, D., (2004), Bond strength comparison of 2 self-etching primers over a 3-month storage period, Am J Orthod Dentofacial Orthop, 126, p709-716.
[https://doi.org/10.1016/j.ajodo.2003.09.032]

-
Turbino, ML., Belan, LC., Soprano, V., Rode, KM., Lloret, PR., Youssef, MN., (2011), Argon ion laser curing depth effect on a composite resin, Lasers Med Sci, 26, p421-425.
[https://doi.org/10.1007/s10103-010-0785-x]

- Uysal, T., Sari, Z., Demir, A., (2004), Are the flowable composites suitable for orthodontic bracket bonding?, Angle Orthod, 74, p697-702.
-
Velo, S., Carano, A., (2002), Self-etching vs. traditional bonding systems in orthodontics: an in vitro study, Orthod Craniofac Res, 5, p166-169.
[https://doi.org/10.1034/j.1600-0544.2002.02193.x]