Comparison of Mechanical Properties of Six Flowable Composite Resins and a Conventional Composite Resin
초록
유동성 레진은 통상적인 복합 레진에 비해 단량체 성분 및 필러 함량이 달라 유동성을 가지므로, 최근 소아치과 분야를 비롯한 치과임상에서 광범위하게 사용되고 있다. 본 연구에서는 6가지 유동성 레진과 1가지 복합 레진의 기계적 성질(굴곡강도, 굴곡계수, 파괴인성,표면조도, 미세경도)를 비교하여 유동성 레진이 치과 임상에서 수복 재료로 사용될 수 있는지를 알아보았다. 유동성 레진으로는 UniFilFlow(UF), UniFil LoFlo Plus(UL), Metafil Flo(MF), Metafil floα(MA), Estelite Flow Quick(EQ), 및 Palfique Esterite LV(PE)를 사용하였고 비교를 위한 복합 레진으로는 Filtek Z350 Universal (FZ)을 사용하였다. 본 연구 결과 UL과 EQ는 복합 레진 FZ에 비해 유의하게 낮은굴곡강도를 나타내었고 (p < 0.05), 모든 유동성 레진이 FZ에 비해 유의하게 낮은 굴곡계수와 파괴인성을 보였다 (p < 0.05). 표면조도는모든 재료에서 유의한 차이가 없었다 (p > 0.05). 특히 유동성 레진은 FZ에 비해 유의하게 낮은 미세경도 값을 나타내어 (p < 0.05) 교합면을포함하는 구치부 수복에는 마모저항성이 문제될 수 있음이 시사되었다. 하지만 교합력이 적은 (약 200 N) 소아 환자에 있어서는 부위에관계 없이 유동성 레진을 이용하여 신속하고 효과적인 수복이 가능할 것으로 생각된다.
키워드:
복합 레진, 유동성 레진, 기계적 성질Ⅰ. INTRODUCTION
Today, restoration using composite resins has increased as esthetic tooth colored alternatives for amalgam and gold inlays. The average annual wear of numerous posterior composite resins is comparable to amalgam. Emphasis on the properties of the flowable composite resins has been put on the flow characteristics of these materials and manufactures have developed them to meet the clinical requirements for improved functionality. The first generation of flowable composite resins was developed in response to requests for easy handling properties in the early 1990s (Baroudi & Rodrigues 2015). Flowable composite resins are low-viscosity resin composites, making them more fluid than universal (conventional) composite resins and provide easy handling property. There are lots of advantages of the flowable composite resins such as (1) high flowability, useful for applying to tooth by means of a small-gage dispenser, especially for those cavities that are not easy to access; (2) ability to form layered structure of minimum thickness to improve or eliminate air inclusion or entrapment; and (3) high flexibility, less likely to be displaced in stress concentration areas (Baroudi & Rodrigues 2015).
As these materials show increased flow characteristics, the filler contents are relatively lower compared to those of the conventional composite resins. They were created mainly by retaining the same small particle size of traditional hybrid composite resins, but reducing the filler content and consequently the viscosity of the mixture. Limited research on flowable resin composites has been undertaken concerning mechanical properties and potential clinical applications.
When flowable resins are also applied for the posterior restorations, much more studies about the properties of the materials are needed for the clinical applications. The purpose of the current study was to evaluate mechanical properties of six commercial flowable composite resins and to compare with those of a conventional composite resin.
Ⅱ. MATERIALS AND METHODS
1. Flexural Properties
Six commercially available flowable and one conventional composite resins were selected for this study. Their characteristics including manufacturers, shades, main compositions, lot numbers are listed in Table 1. A photograph of the materials used is shown in Figure 1.
According to the ISO 4049 specification, a stainless steel split mold was used to prepare flexural property specimens with a dimension of 2 mm × 2 mm × 25 mm. Ten specimens were made for each materials. For light-cured resin specimens, the paste was syringed into the mold, covered by Mylar, and a microscopic slide (1 mm thick) was used to expel extra resin on top of the mold. The specimen was light-cured as specified by the manufacturer, with the curing tip being as close as possible to the Mylar surface, but not touching it, in 5 overlapping sections to ensure maximum conversion on both the top and bottom surfaces, according to ISO 4049. A light-curing unit (Elipar TriLight, 3M ESPE, Seefeld, Germany; standard mode) with 10-mm optic diameter was used. The output intensity of 750 mW/cm2 was constantly monitored during the experiment by a built-in radiometer. Specimens were removed from the mold, trimmed, and stored in distilled water at 37℃ for 24 h before testing.
Flexural properties were then tested using the 3-point bending method with a 20-mm span and a cross-head speed of 0.5 mm/min with a universal testing machine (Model 3343, Instron Inc., Canton, MA, USA). Dimensions of the specimens were determined by a digital caliper. The flexural strength (FS) was calculated using the formula (Lu et al. 2005):
σ = (3Fl)/(2bh2)
where σ is the flexural strength (MPa), F is the load at fracture (N), l is the support span (mm), b is the width (mm), and h is the depth (mm) of the specimen.
The flexural modulus (FM) was calculated using the formula (Lu et al. 2005):
E = [(Fl3)/(δ4bh3)] × 10-3
where E is the flexural modulus (GPa), and F/δ is the slope of the force-displacement curve (N/mm).
2. Fracture Toughness
To determine fracture toughness, single-edge notch specimens were fabricated. A razor blade notch was fixed in a slit of a 5 × 2.5 × 30 mm split mold. The resulting notch/width ratio of the specimen was controlled in the range of 0.45 to 0.55. After resin was packed into the mold and excess was removed, the specimen was exposed to light-polymerization in five 30-s steps on each side. Specimens were removed from the mold, trimmed, and stored in distilled water at 37℃ for 24 h before testing.
At a crosshead speed of 0.1 mm/min, a 3-point bending test was performed on five specimens per composite in a universal testing machine. The stress intensity factor, KQ (MPa√m), was obtained from the peak load and specimen configuration (Kim et al. 2002):
KQ = [(PQ × S)⁄(B × W1.5)] × f(a⁄W)
f(a⁄W) = [3(a⁄W)0.5[1.99−(a⁄W)(1−a⁄W)(2.15−3.93a⁄ W+2.7a2⁄W2)]]/[2(1+2a⁄W)(1−a⁄W)1.5]
where PQ is the peak load (N), S is the span (m), B is the specimen thickness (m), a is the crack length (m), and W is the specimen width (m). The span length was 2 × 10–2 m. As defined by ASTM E-399, if KQ satisfies condition B, a ≥ 2.5 (KQ/σys)2, then KQ may be defined as KIC (fracture toughness) (Kim et al. 2002).
3. Roughness and Microhardness
For roughness and microhardness tests, five specimens per material were collected from the specimens previously subjected to fracture toughness test. The surface roughness was measured using a previously calibrated profilometer (Surftest SV-400, Mitutoyo Corp., Kawasaki, Japan) at a stylus speed of 0.1 mm/s, a cutoff of 0.8 mm, and a range of 600 μm. The Ra of each specimen was recorded as the average of the three readings.
Using a Knoop hardness tester (HMV-2, Shimadzu Corp., Kyoto, Japan), three indentations were made on the top surface of each specimen along a middle line with each indentation separated by approximately 0.5 mm. To make the indentations, a 10-s dwell time and a 25 g load were chosen. The Knoop hardness (KH) of each specimen was recorded as the average of the three readings.
4. Statistical Analysis
Each test parameter was evaluated with one-way analysis of variance (ANOVA). Tukey’s multiple range test was used for post-hoc analysis (p < 0.05).
Ⅲ. RESULTS AND DISCUSSION
1. Flexural Properties
The flexural strengths and flexural moduli of the resin-based composites tested in this study are shown in Table 2. Of the materials, the UL material showed the lowest flexural strength, the difference being statistically significant (p < 0.05). As shown in Table 1, the UF and UL materials had similar chemical compositions (including the filler contents) except for the viscosity. Therefore, it was assumed that the UL materials had a low monomer conversion than the LF materials, thereby produced a significantly lower flexural strength value, although the degrees of conversion were not measured in the present study. Although the other materials exhibited similar flexural strength values, the EQ material, which had a relatively low filler content (Table 1), showed significantly lower values than the rests (p < 0.05).
In ISO 4049:2009(E), Type 1 materials indicate polymerbased restorative materials claimed by the manufacturer as suitable for restorations involving occlusal surfaces. According to the criteria, the use of the UL material was not suitable for restorations involving occlusal surfaces. Instead, the material belonged to Type 2, Class 2 (Group 1), in which the requirement of flexural strength is minimum 50 MPa. Therefore, it can be concluded that all the flowable materials can be used in the posterior regions as well as the anterior regions, except for UL.
The UL material also showed the lowest flexural strength among all the materials tested, the difference being statistically significant (p < 0.05). The PE and FZ materials exhibited significantly higher flexural modulus than the other materials (p < 0.05). Between the two materials, the FZ material showed significantly higher flexural modulus than the PE material. Therefore, in terms of flexural modulus, a conventional composite resin is stiffer than flowable materials (Ryou et al. 2008).
2. Fracture Toughness
In materials science, fracture toughness is a property which describes the ability of a material containing a crack to resist fracture, and is one of the most important properties of any material for many design applications (Abd Wahab et al. 2011). As shown in Table 2, the FZ material showed a significantly higher fracture toughness values than flowable materials (p < 0.05). This finding indicates that flowable composite resins may have weaker fracture resistance than conventional composites (Baroudi & Rodrigues 2015). Therefore, flowable materials should be highly polished without any surface cracks or defects in order to compensate such a drawback (Vichi et al. 2013). In this study, the UL material, which exhibited a low flexural properties, also showed low fracture toughness.
3. Surface Roughness and Microhardness
The surface roughness and microhardness values of the resin-based materials tested are also summarized in Table 2. In this study, there were no significant differences in Ra among the materials tested, indicating that the surfaces prepared against Mylar strip had a similar surface topography.
As shown in Table 2, the conventional composite resin FZ showed a significantly higher microhardness value than the flowable materials (p < 0.05). The hardness of a dental restorative material must be sufficient to resist wear from opposing teeth or restorations and not so hard as to wear enamel and other materials such as porcelain (Wataha & Messer 2004). A restorative material with a low is susceptible to wear, and a hardness greater than enamel may wear existing teeth (Wataha & Messer 2004). The flowable materials appear to have too low microhardness for the use as a restorative material involving occlusal surfaces. Therefore, the formulation of flowable materials should be modified to enhance the microhardness and, as a results, wear resistance (Ryou et al. 2008).
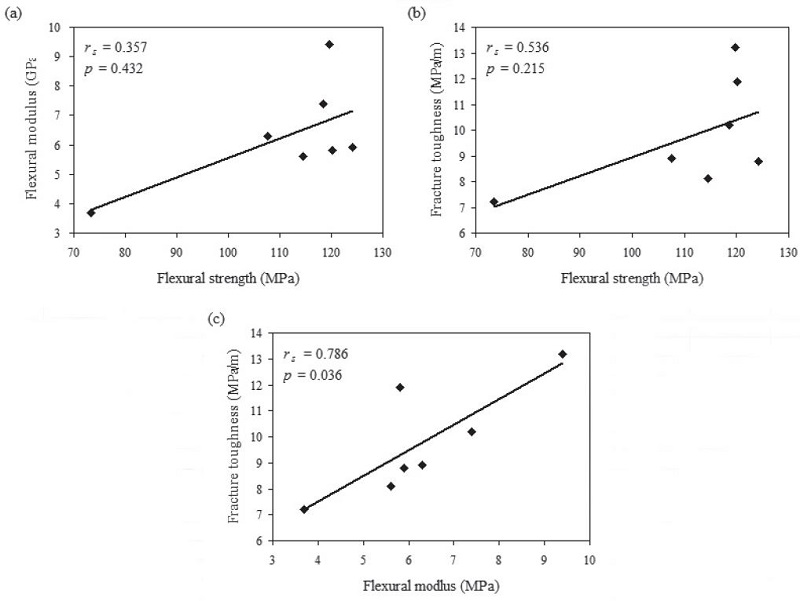
4. Correlations between the Bulk Properties
The parameters of the materials can be divided into two categories: bulk and surface properties. The flexural properties and fracture toughness belong to the former, and the correlations between the properties were evaluated, using Spear correlation analyses (Kim et al. 2014). As shown in Figure 2, there was no significant correlation between the flexural strength and the modulus (a). Similarly, no significant correlation was found between the flexural strength and fracture toughness. In contrast, a significant positive correlation was found between the flexural modulus and fracture toughness. This finding indicate the fracture toughness of a resin-based materials should be evaluated together with the stiffness or flexibility of the material (Liu et al. 2010); further investigations should be performed to confirm this.
Ⅳ. CONCLUSION
The mechanical properties of the flowable composite resins were generally similar or slightly inferior compared with the conventional composite material. However, low fracture toughness and microhardness of the materials suggest that caution should be applied when these materials are used for restorations in the posterior region, in which occlusal loading is significant.
Acknowledgments
This research was supported by Kyungpook National University Research Fund, 2012(2013, 2014).
References
-
Abd Wahab, MH., Bakar, WZ., Husein, A., (2011), Different surface preparation techniques of porcelain repaired with composite resin and fracture resistance, J Conserv Dent, 14, p387-390.
[https://doi.org/10.4103/0972-0707.87207]

-
Baroudi, K., Rodrigues, JC., (2015), Flowable resin composites: A systematic review and clinical considerations, J Clin Diagn Res, 9, pZE18-24.
[https://doi.org/10.7860/jcdr/2015/12294.6129]

- International Organization for Standardization, Dentistry—Polymerbased filling, restorative and luting materials, ISO 4049, (2009).
-
Kim, IH., Park, HS., Kim, YK., Kim, KH., Kwon, TY., (2014), Comparative short-term in vitro analysis of mutans streptococci adhesion on esthetic, nickel-titanium, and stainless-steel arch wires, Angle Orthod, 84, p680-686.
[https://doi.org/10.2319/061713-456.1]

-
Kim, KH., Ong, JL., Okuno, O., (2002), The effect of filler loading and morphology on the mechanical properties of contemporary composites, J Prosthet Dent, 87, p642-649.
[https://doi.org/10.1067/mpr.2002.125179]

-
Liu, Y., Wang, Z., Gao, B., Zhao, X., Lin, X., Wu, J., (2010), Evaluation of mechanical properties and porcelain bonded strength of nickel-chromium dental alloy fabricated by laser rapid forming, Lasers Med Sci, 25, p799-804.
[https://doi.org/10.1007/s10103-009-0690-3]

-
Lu, H., Mehmood, A., Chow, A., Powers, JM., (2005), Influence of polymerization mode on flexural properties of esthetic resin luting agents, J Prosthet Dent, 94, p549-554.
[https://doi.org/10.1016/j.prosdent.2005.09.016]

-
Ryou, DB., Park, HS., Kim, KH., Kwon, TY., (2008), Use of flowable composites for orthodontic bracket bonding, Angle Orthod, 78, p1105-1109.
[https://doi.org/10.2319/013008-51.1]

-
Vichi, A., Margvelashvili, M., Goracci, C., Papacchini, F., Ferrari, M., (2013), Bonding and sealing ability of a new self-adhering flowable composite resin in class I restorations, Clin Oral Investig, 17, p1497-1506.
[https://doi.org/10.1007/s00784-012-0846-6]

-
Wataha, JC., Messer, RL., (2004), Casting alloys, Dent Clin North Am, 48(vii-viii), p499-512.
[https://doi.org/10.1016/j.cden.2003.12.010]