Effect of timing of dentin sealing and provisional restoration method on bond strength of composite resin to dentin

Abstract
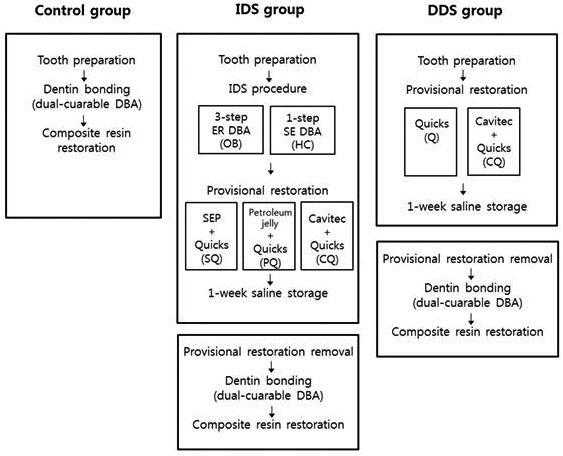
The purpose of this study was to evaluate the effect of timing of dentin sealing and provisional restoration methods on the bond strength of composite resin to dentin. Flat dentin surfaces were prepared and the teeth were divided into three groups: control, resin restoration with immediate dentin sealing (IDS), and resin restoration with delayed dentin sealing (DDS). For the control group, a dentin surface was bonded by using dual-curing dentin adhesive (Excite DSC) and restored with resin immediately. For the IDS groups, a dentin was sealed with OptiBond FL (OB) or Hybrid Coat (HC), and it was restored with following 3 provisional restoration methods: SQ/PQ/CQ {SQ, water-soluble separator (SEP) + provisional resin; PQ, petroleum jelly + provisional resin; CQ, temporary cement (Cavitec) + provisional resin}. For the DDS groups, a dentin was temporized with 2 provisional restoration methods: Q/CQ (Q, provisional resin only) without dentin sealing. After a week, the provisional restoration was removed and cleaned. The treated dentin surface was bonded using Excite DSC and restored with resin, followed by microtensile bond strength (μTBS) tests. The μTBS of control and the IDS-OB groups were not significantly different (P>0.05). The DDS groups presented lower μTBS than control and the IDS-OB groups (P<0.05). The IDS-HC groups were exhibited lowest μTBS than other groups (P<0.05). There was no significant difference in the μTBS regardless of provisional restorative method in the IDS groups (P>0.05). However, using CQ significantly lower the μTBS than using Q in the DDS groups (P<0.05). IDS with a etch-and-rinse type dentin bonding agent improved the bond strength. The use of ZOE-containing cement on the unsealed dentin surface decreased the μTBS.
Keywords:
immediate dentin sealing, delayed dentin sealing, microtensile bond strength, composite resin restoration, provisional restorationⅠ. INTRODUCTION
Successful dentin bonding is particularly important in the case of indirect composite resin restorations such as inlays, onlays, and veneers because the bond strength between teeth and restoration is highly dependent on adhesive procedures (Magne et al., 2005). During the provisional phase or the bonding procedure for indirect restorations, the dentin substrate might be exposed to contaminants, which could reduce the potential of ideal dentin bonding (Hu et al., 2010). Magne et al. reported that freshly cut dentin is the ideal substrate for dentin bonding, suggesting the immediate dentin sealing (IDS) technique rather than delayed dentin sealing (DDS), which has been the preferred conventional method for indirect restoration (Magne et al., 2007).
In IDS technique, dentin bonding agent is followed immediately by cavity preparation prior to taking an impression. With the IDS technique, the clinician can focus on the “wet bonding” to freshly cut dentin, and the sealed dentin is protected from bacterial leakage during temporization (Magne et al., 2005). Consequently, the IDS technique enhances patient comfort by reducing the potential risk of dentin hypersensitivity during temporization, and the cementation procedure requires only limited or no anesthesia, ultimately facilitating occlusal adjustment (Magne et al., 2007). Moreover, this method appears to achieve the increased bond strength, improved restoration adaptation, and fewer gap formations (Stavridakis et al., 2005; Sultana et al., 2007; Udo et al., 2007).
Selecting the dentin adhesive system for dentin sealing is one of the important factors influencing the success of the IDS procedure. A three-step etch-and-rinse (ER) dentin adhesive, especially the filled dentin adhesive, OptiBond FL (OB; Kerr, Orange, CA, USA) has been highly recommended for IDS (Magne et al., 2005; Magne et al., 2007). It is particularly indicated for indirect restoration not only because of the formation of a consistent hybrid layer with resin tags but also because of its cohesiveness with the restorative material (Magne et al., 1999). However, simplification of the clinical procedure for dental restoration is always desirable. Many simplified dentin adhesive systems have been recently introduced to decrease the lengthy and complex application steps and to minimize the technique sensitivity. Hybrid Coat (HC; Sun Medical, Moriyama, Japan) is a one-step self-etch (SE) dentin adhesive, which can be used to seal and protect the adhesive interface between the dentin and the composite resin.
Another concern for the success of indirect restorations is the provisional restorative method. The use of a petroleum jelly as a separator and airborne-particle abrasion with aluminum oxide for surface cleaning before the application of the dentin adhesive has been recommended (Magne et al., 2005). Polishing with pumice or roughening with a coarse diamond rotary instrument at low speed also has been suggested to enhance the bond strength of the composite resin to the dentin with the IDS technique (Magne et al., 2004) Up to now, there are no data comparing the effect of the provisional restorative method after application of a dentin adhesive on bonding effectiveness to composite resin. Thus, the effect of IDS technique and correlation between IDS technique and provisional restoration method on bonding effectiveness of composite resin to dentin should be investigated.
The purpose of this study was to evaluate the bond strength of composite resin to dentin using the IDS technique with different dentin adhesive system and provisional restoration methods. The null hypotheses was that 1) there would be no differences in bond strength of composite resin to dentin according to timing of dentin sealing (IDS vs DDS), 2) there would be no differences in the bond strengths of composite resin to dentin according to the dentin adhesive for IDS, and 3) provisional restoration methods would not influence the bonding efficacy of composite resin to dentin.
Ⅱ. MATERIALS AND METHODS
The chemical composition and the application mode of the dentin adhesives tested in this study are summarized in Table 1.
Twenty-seven extracted human third molars, which had no cavities, cracks or other defects were hand scaled to remove soft tissues and were stored in physiological saline solution. Teeth were embedded in self-curing acrylic resin. After removing the occlusal half of the crown using a model trimmer, the exposed tooth surface was sliced until flat and mid-coronal dentin surface was created using a low-speed diamond saw (MetSAW, MSH-04-112, R&B Inc., Daejeon, Korea) under water cooling. 600-grit silicon carbide paper was used under running water to create a clinically relevant smear layer on the dentin surface.
The teeth were divided into three groups according to the restoration methods: i) immediate resin restoration group (control), ii) delayed resin restoration with IDS treatment (IDS group), and iii) delayed resin restoration without IDS (delayed dentin sealing, DDS) (Table 2).
For the control group, the exposed dentin surface was etched for 15 s with 37.5 % phosphoric acid gel (Etch-37, Bisco Inc., Schaumburg, IL, USA) followed by abundant rinse and blot air dry. Dual-curing dentin adhesive (Excite DSC; IvoclarVivadent, Schaan, Liechtenstein) was applied for 15 s and air-dried for 5 s followed by light polymerization for 20 s with an Optilux 501 halogen curing light (Kerr, Middleton, WI, USA) with an energy higher than 450 mW/cm2 as measured by a curing radiometer (Optilux Radiometer; Kerr, Middleton, WI, USA). Estelite composite resin (Tokuyama Dental Corp, Tokyo, Japan), shade A2, was built up on the treated dentin surface to 4 mm high in increments of 2 mm; each increment was light cured for 20 s.
For the IDS groups, the dentin surface was sealed with two dentin adhesives according to the manufacturer’s instructions: i) three-step etch-and-rinse system (OB) and ii) one-step SE dentin adhesive (HC). The prepared dentin surfaces were restored with one of the following three provisional restorative methods: i) SQ method, water-soluble separator (SEP; Superbond SEP, Sun Medical, Moriyama, Japan) + provisional composite resin (Quicks; Denkist, Seoul, Korea), ii) PQ method, petroleum jelly + Quicks, and iii) CQ method, temporary cement (Cavitec; Kerr, Orange, CA, USA) + Quicks. For SQ and PQ method, the thin coat of SEP and petroleum jelly were applied to the sealed dentin surface. Quicks was built up until it was 2 mm high and light cured for 40 s, followed by one-week saline storage. For CQ method, pre-cured Quicks in 2mm-height was cemented with Cavitec.
For the DDS groups, the dentin surface was restored with two different provisional restorative methods without applying the dentin adhesive: i) Q method, Quicks only and ii) CQ method, Cavitec+ Quicks. For Q method, Quick was applied without any dentin surface treatment. For CQ method, the dentin surface was temporalized as same as CQ method in IDS group.
For the IDS and DDS groups, the specimens were kept in saline for one week. Then, the provisional restoration was removed and the sealed dentin was cleaned by water and fluoride-free pumice (Zircate Prophy Paste, Denstply Caulk, Milford, DE, USA). A dentin adhesive, Excite DSC, was applied, followed by 4-mm-high composite resin restoration using Estelite in 2-layer increments.
All the specimens were then stored in 100% humidity for 24 h at 37°C. After 24 h storage, the teeth were sectioned in the X and Y perpendicular directions with a low-speed diamond saw in order to obtain multiple beams with cross-sectional areas of approximately 0.81 mm2 for the microtensile bond strength (μTBS) test. Approximately 11 to 13 beams were prepared from each tooth, and four of beams among them were selected to include the specimen with similar length and proportion of dentin-composite complex. The ends of each specimen were fixed to the microtensile tester (Bisco Inc., Schaumburg, IL, USA) with cyanoacrylate adhesive plus an accelerator (Zapit® base and accelerator, Dental Ventures of America Inc., CA, USA). μTBS test was carried out at a crosshead speed of 1mm/min until failure occurred. The results were obtained at the moment of the specimen fracture and calculated in MPa.
The μTBS data were statistically analyzed by two-way analysis of variance (ANOVA). The Tukey HSD test was used to detect pairwise differences among experimental groups. All statistical testing was performed at a preset alpha of 0.05. Statistical analysis was performed using SPSS for Windows (version 12.0; IBM SPSS Inc., Chicago, IL, USA).
Ⅲ. RESULTS
Table 3 shows the μTBS values for each group. The μTBS of control and the IDS-OB groups presented highest μTBS, and there were no significant difference (P>0.05). There was no significant difference in the μTBS values between the IDS-OB groups according to the provisional restorative method (P>0.05). The IDS-HC groups were exhibited lowest μTBS than other groups (P<0.05). Within the IDS-HC groups, no significant differences were observed according to the provisional restorative method (P>0.05). The DDS groups presented lower μTBS than control and the IDS-OB groups (P<0.05). Within the DDS groups, using CQ significantly lower the μTBS than using Q for provisional restorative method (P<0.05).
Ⅳ. DISCUSSION
Magne et al. suggested that when preparing teeth for indirect bonded restorations using the IDS technique, because of the delayed placement of the restoration and postponed occlusal loading, the dentin bond can increase over time and residual stresses can dissipate, resulting in significantly improved restoration adaptation. (Magne et al., 2005) IDS technique is mostly used in indirect restoration, and the bonded dentin surface is luted using resin cement followed by seating the indirect restoration. To investigate the bonding effectiveness of IDS technique on dentin to composite, Magne et al used dentin/restoration complex model instead of dentin/cement/indirect restoration complex model to reduce the procedural errors which can be happened between multiple adhesive interfaces (Magne et al., 2005, Magne et al., 2007). In this study, we also used dentin/restoration complex model to evaluate the effect of IDS technique and correlation between IDS technique and provisional restoration method on bond strengths of composite resin to dentin.
Several studies incorporating various dentin adhesives and application methods have also shown that the IDS technique showed increased adhesive effectiveness as compared to the DDS technique, which is related to formation of longer resin tags and a thicker hybrid zone on the freshly cut dentin (Jayasooriya et al., 2003; Okuda et al., 2007). Moreover, the IDS technique can protect the tooth from the consequences of microleakage by sealing the dentinal tubules that are vulnerable to bacterial invasion immediately after completion of the preparation (Demirci et al., 2013; Magne et al., 2005). Sealing the dentin tubules also reduces sensitivity by preventing hydraulic fluid flow within the dentin tubules, which is associated with postoperative sensitivity (Suzuki et al., 1994).
Postoperative dentin hypersensitivity is one of the nuisances that dentists frequently confront in a clinical situation. HC is originally introduced to the market as desensitization agent which could be also used as dentin adhesive; thus it might be an easy, fast and user-friendly material during temporalization period. However, the IDS groups with three-step ER dentin adhesive (OB) showed significantly higher bond strengths than the IDS groups with one-step SE dentin adhesive (HC) and the DDS groups. Thus, the first null hypothesis was partially rejected and the second one was rejected.
As reported in several studies, most simplified one-step SE dentin adhesive are the least durable, whereas three-step etch-and-rinse and two-step SE dentin adhesive continue to show the best performance in terms of bond strength, aging, and stability of the bonded interface (Mine et al., 2009; Sarr et al., 2010; Scholtanus et al., 2010). One-step SE dentin adhesive has been shown to contain a higher concentration of acid derivatives, methacrylated phosphoric acid esters, water, and organic solvents than conventional dentin adhesives, simultaneously etching and infiltrating the dentin surface. HC is a one-step SE dentin adhesive comprising 4-methacyloxyethyl trimellitic anhydride (4-META) as a functional acidic monomer that decalcifies dentin substrate and penetrates through the smear layer to form a hybrid layer. However, the low pH (1.5–2.5) of one-step SE dentin adhesive due to the acidic monomers makes them hydrolytically unstable and permeable because of the mixture of methacrylate-based components and hydrophilic components (Nayif et al., 2010). The adhesive interfaces of the one-step SE dentin adhesive differed significantly as compared to other multi-step adhesive systems that form a thin and irregular adhesive layer (Nayif et al., 2010; Van Landuyt et al., 2009). Concerning the thickness of the oxygen inhibition layer, the thin adhesive layer of one-step SE dentin adhesive might also affect from low degrees of conversion, thus reducing the quality of the adhesive interface (Amirouche-Korichi et al., 2009). Considering the above, multi-step adhesive systems, including the separated hydrophobic bonding component, are appropriate for IDS because of their ability to form a more hydrophobic and uniform resin coating.
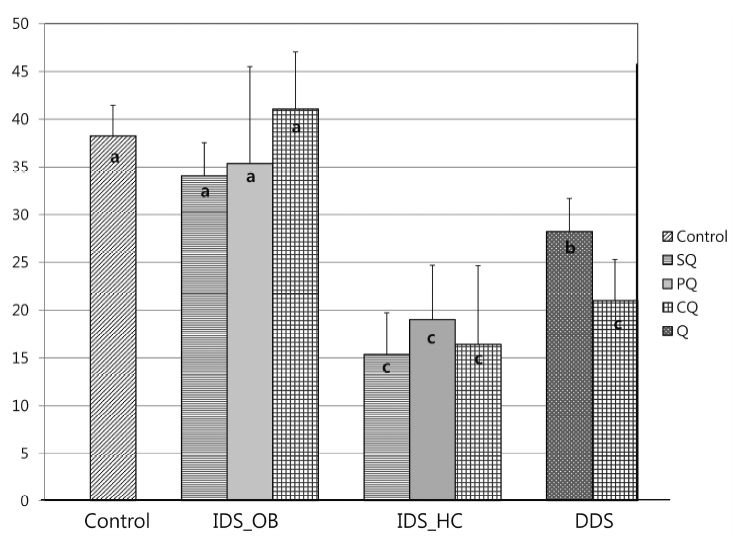
Microtensile bond strength of experimental groups (MPa)Abbreviations, IDS: immediate dentin sealing, OB: OptiBond FL, HC: Hybrid Coat, DDS: delayed dentin sealing, SQ: water-soluble separator (SEP) + provisional composite resin (Quicks), PQ: petroleum jelly + Quicks, CQ: ZOE-based temporary cement (Cavitec) + Quicks, Q: Quicks only. Different superscript indicates a significant difference (P<0.05).
Practically speaking, provisional restorative methods for indirect restoration need to be used with caution because the IDS-treated surfaces have the potential to bond to resin-based provisional materials and cements. Considering that the IDS technique can be used not only for inlays and onlays but also for full veneer crowns, the influence of provisional cement on dentin bonding is another important issue. In our study, there was no significant difference in the μTBS regardless of provisional restorative method so that third null hypothesis was rejected.
Among the contemporary dental materials, zinc oxide eugenol (ZOE) is presumably one of the most popular provisional cements for indirect restorations because it is easy to remove, cost effective, and it has a sedative effect on hypersensitivity (Kielbassa et al., 1997; Markowitz et al., 1992). However, the use of ZOE-containing provisional cements has to be considered carefully prior to definitive adhesive cementation with dentin adhesives and resin cements (Carvalho et al., 2007; Frankenberger et al., 2007; Yap et al., 2001). The polymerization of composite resins and dentin adhesives is induced by radicals; however, eugenol is a radical scavenger that inhibits the polymerization reaction (Hume, 1984). The hydroxyl group of the eugenol molecule tends to protonize these radicals and blocking their reactivity and reduce the degree of conversion of the composite (Kielbassa et al., 1997). In the present study, there was no significant difference in the IDS groups according to the provisional restoration method. However, using Cavitec with provisional restoration statistically significantly lower the bond strength in the DDS groups (P<0.05). In previous studies, ZOE-containing cements could be used safely prior to inserting resin-based filling materials (Carvalho et al., 2007; Peutzfeldt et al., 2006). On the other hand, there are contradictory findings mentioning that ZOE-containing cements should be avoided because of the detrimental effect on bonding (Millstein et al., 1992; Xie et al., 1993). According to the in vitro experimental model by Hume, the effect of eugenol concentration on dentin remains relatively constant for more than a week because of the release and diffusion action of eugenol through the dentin (Hume, 1984). Although the methodology used in current study has limited ability in terms of analyzing the cause of different results of bond strength, we speculate that eugenol might remain an adherent surface due to the diffusion through the dentin in the DDS group, thus affecting the bond strength results.
A key element in IDS is the development of an efficient resin-to-resin bond between the existing resin coating by dentin adhesive and the new composite resin cement. In clinical situation, IDS technique is the application of a dentin adhesives followed by cavity preparation prior to making an impression for indirect restoration. In our study, we performed not indirect restoration with composite resin cement but direct resin restoration on the IDS or DDS surface with dual-curing dentin adhesive. Our experimental design was followed the previous study (Magne et al., 2007). This situation is somewhat similar to a resin-to-resin repair, and so surface conditioning methods can influence the bond strength. By simplifying the experimental procedure, we can rule out the procedural errors during the cementation procedure or bias from the indirect restoration material such as type of ceramic and composite resin. Additionally, recent trend in the cementation of indirect restoration is the use of self-adhesive resin cement which has advantage in its convenience. It has been reported that there are no significant differences between various self-adhesive resin cements, and those results were clinically favorable to use (Kim et al., 2013). Bonding effectiveness of self-adhesive resin cement with IDS treated dentin surface should be further investigated to determine its clinical application.
Although Magne et al. recommend to use airborneparticle abrasion with aluminum oxide for surface conditioning (Magne et al., 2005; Magne et al., 2007), we used fluoride-free pumice IDS and DDS surfaces. Recent study has reported that there is no significant difference in fluoride-free pumice paste, airborne-particle abrasion with aluminum oxide, or glycin (Falkensammer et al., 2014). In our study, we did not aim to compare the effect of surface conditioning method on bonding efficacy of dentin to composite. However, different surface conditioning method might influence the surface morphology or bonding efficacy. Further study on surface conditioning on IDS surface is necessary for final evaluation of the suggested results.
Ⅴ. CONCLUSION
We found that sealing the dentin with a three-step etch-and-rinse system prior to provisional restoration in indirect resin restoration resulted in improved bond strength. Using the IDS technique for indirect restoration, provisional restorative methods did not decrease the bond strength to the composite resin. However, without using the IDS technique, the use of a ZOE-containing provisional cement may be contraindicated because of reduction of bond effectiveness.
Acknowledgments
The authors declare no conflict of interest and no source of funding.
Ⅵ. REFERENCES
-
Amirouche-Korichi, A., Mouzali, M., Watts, DC., (2009), Effects of monomer ratios and highly radiopaque fillers on degree of conversion and shrinkage-strain of dental resin composites, Dent Mater, 25, p1411-1418.
[https://doi.org/10.1016/j.dental.2009.06.009]

-
Carvalho, CN., de Oliveira Bauer, JR., Loguercio, AD., Reis, A., (2007), Effect of ZOE temporary restoration on resin-dentin bond strength using different adhesive strategies, J Esthet Restor Dent, 19, p144-152.
[https://doi.org/10.1111/j.1708-8240.2007.00087.x]

-
Demirci, M., Tuncer, S., Tekce, N., Erdilek, D., Uysal, O., (2013), Influence of adhesive application methods and rebonding agent application on sealing effectiveness of all-in-one self-etching adhesives, J Esthet Restor Dent, 25, p326-343.
[https://doi.org/10.1111/jerd.12034]

-
Falkensammer, F., Arnetzl, GV., Wildburger, A., Krall, C., Freudenthaler, J., (2014), Influence of different conditioning methods on immediate and delayed dentin sealing, J Prosthet Dent, 112, p204-210.
[https://doi.org/10.1016/j.prosdent.2013.10.028]

- Frankenberger, R., Lohbauer, U., Taschner, M., Petschelt, A., Nikolaenko, SA., (2007), Adhesive luting revisited: influence of adhesive, temporary cement, cavity cleaning, and curing mode on internal dentin bond strength, J Adhes Dent, 9, p269-273.
- Hu, J., Zhu, Q., (2010), Effect of immediate dentin sealing on preventive treatment for postcementation hypersensitivity, Int J Prosthodont, 23, p49-52.
-
Hume, WR., (1984), An analysis of the release and the diffusion through dentin of eugenol from zinc oxide-eugenol mixtures, J Dent Res, 63, p881-884.
[https://doi.org/10.1177/00220345840630061301]

-
Jayasooriya, PR., Pereira, PN., Nikaido, T., Tagami, J., (2003), Efficacy of a resin coating on bond strengths of resin cement to dentin, J Esthet Restor Dent, 15, p105-113.
[https://doi.org/10.1111/j.1708-8240.2003.tb00325.x]

- Kielbassa, AM., Attin, T., Hellwig, E., (1997), Diffusion behavior of eugenol from zinc oxide-eugenol mixtures through human and bovine dentin in vitro, Oper Dent, 22, p15-20.
- Kim, AJ., Yu, SH., Oh, SH., Bae, JM., (2013), 자가 접착 레진 시멘트의 전단결합강도, 굴곡강도, 물 흡수도 및 용해도, Kor J Dent Mater, 40, p57-64.
-
Magne, P., (2005), Immediate dentin sealing: a fundamental procedure for indirect bonded restorations, J Esthet Restor Dent, 17, p144-154.
[https://doi.org/10.1111/j.1708-8240.2005.tb00103.x]

-
Magne, P., Belser, UC., (2004), Novel porcelain laminate preparation approach driven by a diagnostic mock-up, J Esthet Restor Dent, 16, p7-16.
[https://doi.org/10.1111/j.1708-8240.2004.tb00444.x]

- Magne, P., Douglas, WH., (1999), Porcelain veneers: dentin bonding optimization and biomimetic recovery of the crown, Int J Prosthodont, 12, p111-121.
-
Magne, P., Kim, TH., Cascione, D., Donovan, TE., (2005), Immediate dentin sealing improves bond strength of indirect restorations, J Prosthet Dent, 94, p511-519.
[https://doi.org/10.1016/j.prosdent.2005.10.010]

-
Magne, P., So, WS., Cascione, D., (2007), Immediate dentin sealing supports delayed restoration placement, J Prosthet Dent, 98, p166-174.
[https://doi.org/10.1016/S0022-3913(07)60052-3]

-
Markowitz, K., Moynihan, M., Liu, M., Kim, S., (1992), Biologic properties of eugenol and zinc oxide-eugenol. A clinically oriented review, Oral Surg Oral Med Oral Pathol, 73, p729-737.
[https://doi.org/10.1016/0030-4220(92)90020-Q]

-
Millstein, PL., Nathanson, D., (1992), Effects of temporary cementation on permanent cement retention to composite resin cores, J Prosthet Dent, 67, p856-859.
[https://doi.org/10.1016/0022-3913(92)90601-6]

-
Mine, A., De Munck, J., Cardoso, MV., Van Landuyt, KL., Poitevin, A., Kuboki, T., Van Meerbeek, B., (2009), Bonding effectiveness of two contemporary self-etch adhesives to enamel and dentin, J Dent, 37, p872-883.
[https://doi.org/10.1016/j.jdent.2009.06.020]

- Nayif, MM., Shimada, Y., Ichinose, S., Tagami, J., (2010), Nanoleakage of current self-etch adhesives bonded to artificial carious dentin, Am J Dent, 23, p279-284.
-
Okuda, M., Nikaido, T., Maruoka, R., Foxton, RM., Tagami, J., (2007), Microtensile bond strengths to cavity floor dentin in indirect composite restorations using resin coating, J Esthet Restor Dent, 19, p38-46.
[https://doi.org/10.1111/j.1708-8240.2006.00062.x]

- Peutzfeldt, A., Asmussen, E., (2006), Influence of eugenolcontaining temporary cement on bonding of selfetching adhesives to dentin, J Adhes Dent, 8, p31-34.
-
Sarr, M., Kane, AW., Vreven, J., Mine, A., Van Landuyt, KL., Peumans, M., De Munck, J., (2010), Microtensile bond strength and interfacial characterization of 11 contemporary adhesives bonded to bur-cut dentin, Oper Dent, 35, p94-104.
[https://doi.org/10.2341/09-076-L]

- Scholtanus, JD., Purwanta, K., Dogan, N., Kleverlaan, CJ., Feilzer, AJ., (2010), Microtensile bond strength of three simplified adhesive systems to caries-affected dentin, J Adhes Dent, 12, p273-278.
- Stavridakis, MM., Krejci, I., Magne, P., (2005), Immediate dentin sealing of onlay preparations: thickness of pre-cured Dentin Bonding Agent and effect of surface cleaning, Oper Dent, 30, p747-757.
-
Sultana, S., Nikaido, T., Matin, K., Ogata, M., Foxton, RM., Tagami, J., (2007), Effect of resin coating on dentin bonding of resin cement in Class II cavities, Dent Mater J, 26, p506-513.
[https://doi.org/10.4012/dmj.26.506]

- Suzuki, S., Cox, CF., White, KC., (1994), Pulpal response after complete crown preparation, dentinal sealing, and provisional restoration, Quintessence Int, 25, p477-485.
-
Udo, T., Nikaido, T., Ikeda, M., Weerasinghe, DS., Harada, N., Foxton, RM., Tagami, J., (2007), Enhancement of adhesion between resin coating materials and resin cements, Dent Mater J, 26, p519-525.
[https://doi.org/10.4012/dmj.26.519]

- Van Landuyt, KL., Mine, A., De Munck, J., Jaecques, S., Peumans, M., Lambrechts, P., Van Meerbeek, B., (2009), Are one-step adhesives easier to use and better performing? Multifactorial assessment of contemporary one-step self-etching adhesives, J Adhes Dent, 11, p175-190.
-
Xie, J., Powers, JM., McGuckin, RS., (1993), In vitro bond strength of two adhesives to enamel and dentin under normal and contaminated conditions, Dent Mater, 9, p295-299.
[https://doi.org/10.1016/0109-5641(93)90046-S]

- Yap, AU., Shah, KC., Loh, ET., Sim, SS., Tan, CC., (2001), Influence of eugenol-containing temporary restorations on bond strength of composite to dentin, Oper Dent, 26, p556-561.